GI Bleed Risk Calculator for Antiplatelet Therapy
Your Risk Factors
Your Antiplatelet Therapy
Risk Assessment Results
PPI Recommendations
- Recommended
- Avoid
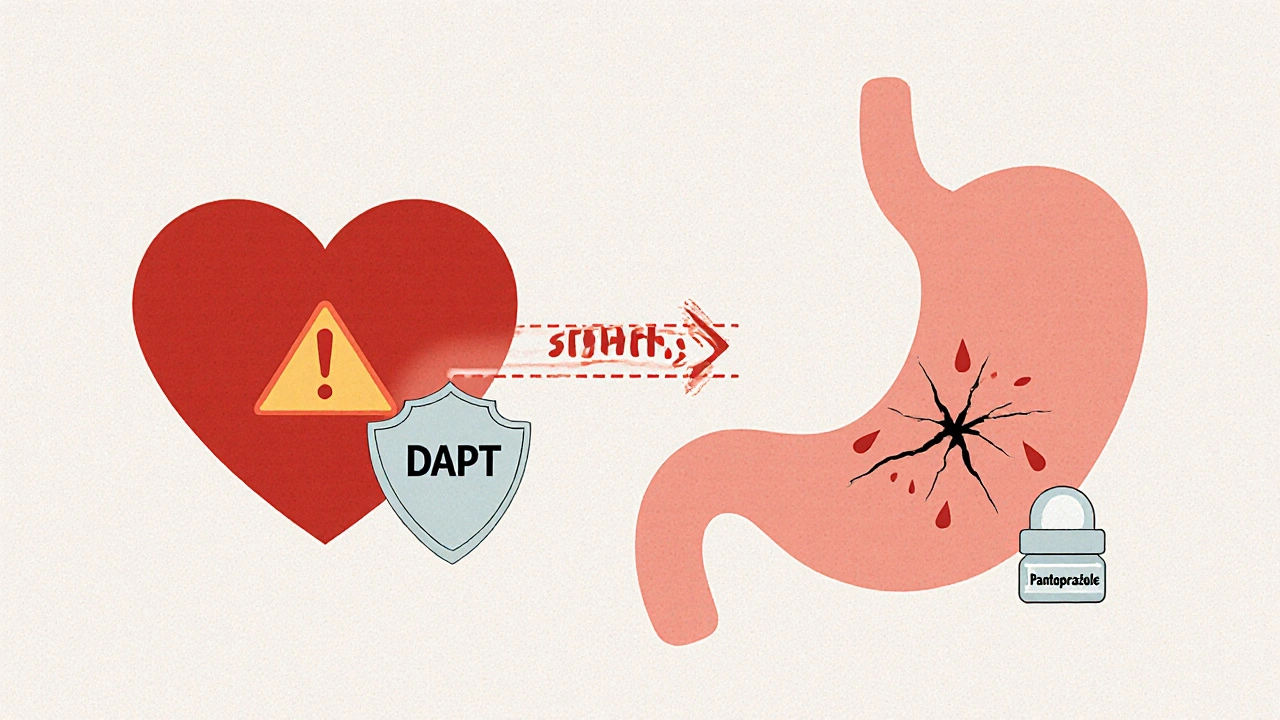
When you’re on dual antiplatelet therapy - usually aspirin plus clopidogrel, prasugrel, or ticagrelor - your blood doesn’t clot as easily. That’s good for preventing heart attacks and strokes. But it also means your stomach is more vulnerable. Every year, tens of thousands of people on these drugs suffer dangerous gastrointestinal (GI) bleeding. The good news? Adding a proton pump inhibitor (PPI) can slash that risk by nearly 40%. The bad news? Many doctors still get it wrong - either prescribing the wrong PPI, giving it to people who don’t need it, or skipping it altogether when they should.
Why Dual Antiplatelet Therapy Increases GI Bleed Risk
Dual antiplatelet therapy (DAPT) is standard after a heart attack, stent placement, or stroke. It combines aspirin with a P2Y12 inhibitor like clopidogrel. Together, they block platelets from clumping, which keeps arteries open. But aspirin also irritates the stomach lining. It reduces protective mucus and lets stomach acid eat away at tissue. Add in the other antiplatelet drugs, and the risk of bleeding shoots up by 30-50% in the first month. By six months, about 1 in 20 patients on DAPT will have a serious GI bleed. That’s not rare. It’s common enough that guidelines now treat it as an expected side effect - not an accident.How PPIs Protect Your Stomach
Proton pump inhibitors like omeprazole, esomeprazole, and pantoprazole shut down the acid pumps in your stomach lining. They don’t just reduce acid - they cut it by 70% to 98%. That gives your stomach time to heal. Studies show that when you take a PPI with DAPT, your chance of a major GI bleed drops by 34-37%. In one study of nearly 97,000 stroke patients, those on PPIs had a 37% lower risk of serious bleeding over a year. That’s not a small benefit. It’s life-saving.Not All PPIs Are Created Equal
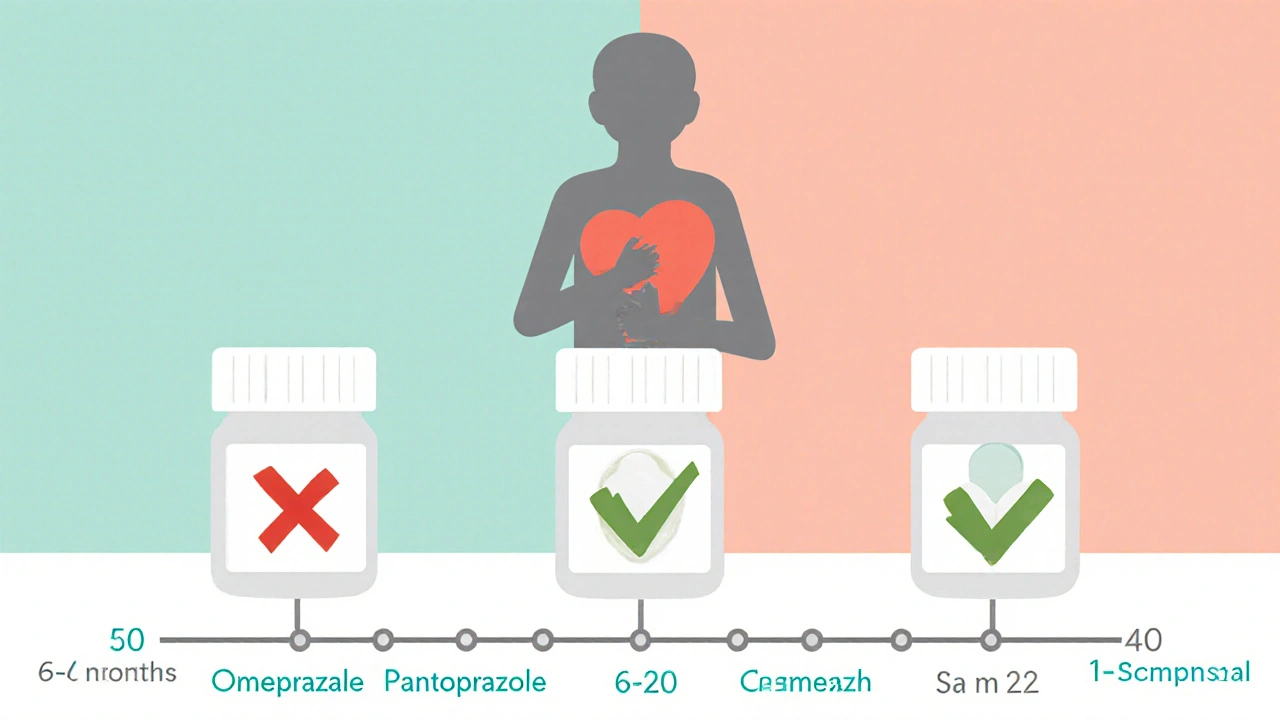
Here’s where things get tricky. Omeprazole is cheap and widely used. But it interferes with clopidogrel. Clopidogrel needs to be activated by an enzyme called CYP2C19. Omeprazole blocks that enzyme. In lab tests, it cuts clopidogrel’s effectiveness by up to 45%. That means more heart attacks. The COGENT trial found that patients on omeprazole and clopidogrel had a 27% higher risk of cardiovascular events compared to those on other PPIs.Pantoprazole and esomeprazole don’t do this. They barely touch CYP2C19. If you’re on clopidogrel, these are the only PPIs you should take. Pantoprazole 40 mg daily is the top choice. Esomeprazole 40 mg daily works too - especially if you’re on ticagrelor or prasugrel, since those drugs don’t rely on CYP2C19. Don’t use omeprazole with clopidogrel. Ever. It’s not a close call. It’s a known danger.
PPIs vs. H2 Blockers: Why PPIs Win
Some doctors try to cut costs by switching to famotidine or ranitidine - H2 receptor antagonists. They reduce acid, but not enough. A 2017 meta-analysis found PPIs cut GI bleeding risk by 60%. H2 blockers? Only 30%. That’s half the protection. And when you’re on DAPT, half isn’t enough. In real-world terms: for every 100 patients on DAPT, PPIs prevent 1.8 major bleeds. H2 blockers prevent 0.9. That’s the difference between a near-certainty of safety and a gamble.Who Actually Needs a PPI?
Not everyone on DAPT needs a PPI. But too many get one anyway. The 2023 European Society of Cardiology guidelines say: give a PPI if you have two or more of these risk factors:- History of GI bleeding or ulcers
- Age 65 or older
- Taking blood thinners like warfarin or apixaban
- Using NSAIDs (ibuprofen, naproxen)
- On corticosteroids
If you’re 50, healthy, no prior bleeding, no other meds - you probably don’t need it. But here’s the problem: a 2022 study found 35-45% of DAPT patients on PPIs had no risk factors. That’s overprescribing. And it’s dangerous. Long-term PPI use raises your risk of C. diff infection, pneumonia, and even chronic kidney disease. It’s not harmless. It’s a tool. Use it only when needed.
When to Start - And When to Stop
Start the PPI on day one of DAPT. Most GI bleeds happen in the first 30 days. Waiting until you feel pain? Too late. The damage is already done.How long should you take it? For most people, 6 to 12 months is enough. After that, your bleeding risk drops sharply. If you’re still on DAPT beyond a year - maybe because you had a second heart attack or multiple stents - keep the PPI. But if your doctor wants to keep you on it for years without reassessing? Push back. Ask: Do I still have two or more risk factors? If not, it’s time to stop.
The Hidden Problem: Underuse and Overuse
There’s a gap in care. In Korea, a 2025 study found only 16.6% of low-risk DAPT patients got a PPI - even though they had clear benefit. Meanwhile, in the U.S., nearly half of PPI prescriptions for DAPT patients had no valid reason. That’s underuse in some places, overuse in others. The result? More bleeding where it could’ve been prevented. More infections where it wasn’t needed.One reason? Doctors aren’t sure who qualifies. A 2022 survey showed 45% of cardiologists felt unsure about when to prescribe. Another? Patients hate taking extra pills. One in three worry about polypharmacy. But the math is simple: one pill to prevent a hospital stay, a blood transfusion, or surgery? That’s worth it.
What’s Coming Next
New drugs are on the horizon. Vonoprazan, a potassium-competitive acid blocker, is coming to the U.S. in late 2025. It blocks acid even better than PPIs - and doesn’t touch CYP2C19. No interaction with clopidogrel. No increased heart risk. It’s the ideal solution. But it’s not here yet. Until then, use pantoprazole or esomeprazole.Genetic testing is also emerging. Some people have a CYP2C19 gene variant that makes clopidogrel less effective. If you’re one of them, you might need a different antiplatelet - or a different PPI. Mayo Clinic is already testing this in high-risk patients. By 2027, genotype-guided prescribing could become standard.
What You Should Do Right Now
If you’re on DAPT:- Ask your doctor: Which PPI am I on? If it’s omeprazole, ask if you can switch to pantoprazole or esomeprazole.
- Ask: Do I have two or more risk factors? If yes, you need it. If no, ask why you’re taking it.
- Ask: How long do I need to take this? Most people only need 6-12 months.
- Don’t take NSAIDs like ibuprofen. They double your bleeding risk. Use acetaminophen instead for pain.
- Don’t stop your PPI without talking to your doctor. Abruptly stopping can cause rebound acid and ulcers.
The goal isn’t to avoid all meds. It’s to use the right ones, at the right time, for the right person. PPIs with antiplatelets isn’t a combo you take because it’s trendy. It’s a lifesaving strategy - if done right.
Can I take omeprazole with clopidogrel?
No. Omeprazole reduces clopidogrel’s effectiveness by up to 45% by blocking the CYP2C19 enzyme your body needs to activate it. This increases your risk of heart attack or stroke. Use pantoprazole or esomeprazole instead. They don’t interfere with clopidogrel.
Do I need a PPI if I’m on ticagrelor or prasugrel?
Yes - if you have risk factors for GI bleeding. Ticagrelor and prasugrel don’t rely on CYP2C19, so you can safely use any PPI, including omeprazole. But pantoprazole and esomeprazole are still preferred because they’re proven effective and have the best safety record. Don’t skip the PPI just because your antiplatelet is newer - your stomach still needs protection.
How long should I take a PPI with DAPT?
Most people need it for 6 to 12 months. That’s when the risk of GI bleeding is highest. After that, the risk drops significantly. If you’re still on DAPT beyond a year (for example, after multiple stents or a second heart event), continue the PPI. But if your risk factors are gone - like you’re no longer on NSAIDs or you’re under 65 with no prior bleeding - ask your doctor about stopping it.
Can PPIs cause long-term harm?
Yes - if taken unnecessarily for years. Long-term use is linked to higher risk of C. diff infection, pneumonia, kidney disease, and bone fractures. The FDA has issued warnings about these risks. That’s why guidelines stress using PPIs only when you have two or more risk factors. Don’t take it just because you were prescribed it once. Reassess every 6-12 months.
Is it safe to take a PPI with aspirin only?
Only if you have a history of ulcers or GI bleeding. Aspirin alone increases GI bleeding risk 2-4 times compared to placebo. If you’re on low-dose aspirin for heart protection and have no prior bleeding, you probably don’t need a PPI. But if you’ve had a bleed before, even on aspirin alone, you should be on a PPI long-term. Always talk to your doctor - don’t assume.


Olanrewaju Jeph
November 23, 2025 AT 14:29Great breakdown. I’ve been on clopidogrel for two years after a stent, and my cardiologist switched me from omeprazole to pantoprazole last year after I mentioned the interaction. No more heartburn, and my last blood test showed normal platelet activity. Always ask about the PPI - it’s not just a stomach pill, it’s part of your cardiac safety net.
Dalton Adams
November 23, 2025 AT 20:13Let’s be real - most GPs don’t even know CYP2C19 exists. I work in pharma R&D, and I’ve seen the data. Omeprazole is a relic. It’s like prescribing leeches with aspirin. Pantoprazole? Yes. Esomeprazole? Also yes. Vonoprazan? Coming soon, and it’ll make PPIs look like medieval medicine. Also, stop using NSAIDs. Ibuprofen is just liquid bleeding. Acetaminophen is your new best friend. And yes, I’ve published on this. You’re welcome.
Kane Ren
November 25, 2025 AT 05:41This is the kind of info that actually saves lives. I was terrified after my heart attack, but knowing I could protect my stomach without hurting my heart? Huge relief. My doc didn’t even mention PPIs at first - I had to bring it up. Don’t wait for them to tell you. Ask. Advocate. You’ve got this.
Charmaine Barcelon
November 26, 2025 AT 09:15Okay, but… did you know? PPIs can cause kidney damage? And pneumonia? And bone fractures? And C. diff? So… if you don’t have two risk factors? STOP. NOW. Seriously. You’re not helping yourself. You’re just making your body a playground for side effects. I’ve seen it. Too many times. Please, just… stop.
Karla Morales
November 27, 2025 AT 10:44📊 Data point: 35–45% of DAPT patients on PPIs have zero risk factors. 📉 That’s not clinical practice - that’s autopilot prescribing. 🧬 And CYP2C19 polymorphism? We’re already in the era of pharmacogenomics. If your doctor hasn’t mentioned genetic testing… they’re 5 years behind. 🏥 #PharmaAwareness #DAPT #PPIsAreNotCandy
Javier Rain
November 28, 2025 AT 21:04I’m a nurse, and I’ve seen patients bleed out from GI bleeds because no one told them about PPIs. Or worse - they got omeprazole and had a second heart attack. This isn’t theoretical. It’s real. If you’re on dual therapy, don’t wait for symptoms. Start the right PPI on day one. And if your doc says "it’s fine," ask for the guidelines. They’re right there in black and white. You deserve better.
Laurie Sala
November 29, 2025 AT 20:02I’ve been on PPIs for 7 years… and now I have chronic kidney disease. I didn’t know it was linked. My doctor just kept refilling it. I thought it was "just for my stomach." I feel so stupid. I’m 52, no ulcers, no NSAIDs… why did I take it for so long? I wish someone had told me this sooner. I’m crying now.
Lisa Detanna
December 1, 2025 AT 12:15In Nigeria, we don’t even have access to pantoprazole in many rural clinics. Omeprazole is all there is. And clopidogrel? Often imported without proper guidance. This isn’t just a U.S. problem - it’s a global health equity issue. We need education, not just prescriptions. Maybe someone can start a WHO initiative? We can’t keep sacrificing stomachs for hearts - especially when the tools exist.
Demi-Louise Brown
December 1, 2025 AT 14:45Start PPI on day one. Stop after 12 months unless you have two risk factors. Use pantoprazole or esomeprazole. Avoid NSAIDs. Reassess annually. Simple. Clear. Evidence-based. This is how medicine should work.