Corticosteroid Psychosis Risk Calculator
How This Tool Works
This calculator estimates your risk of developing psychiatric side effects from corticosteroids based on key factors. It's designed to help you and your healthcare provider identify potential risks early. Remember: this is for informational purposes only and not a substitute for professional medical advice.
When Steroids Change Your Mind
Most people know corticosteroids help with inflammation, asthma, or rheumatoid arthritis. But few realize these powerful drugs can also change how you think, feel, and act - sometimes in dangerous ways. Up to 18% of people taking high doses of steroids like prednisone develop serious psychiatric symptoms, including hallucinations, paranoia, and full-blown psychosis. This isn’t rare. It’s common enough that doctors should be watching for it from day one.
How Common Is Steroid-Induced Psychosis?
Every year in the U.S. alone, doctors write about 10 million prescriptions for oral corticosteroids. That’s millions of people exposed to a drug that can trigger mental health crises. The risk isn’t the same for everyone. At doses under 40 mg of prednisone per day, about 1.3% of patients experience psychiatric side effects. But jump to 80 mg or higher, and that number spikes to nearly 1 in 5. Even at moderate doses, mood swings, insomnia, and irritability show up in over a third of users.
The worst cases - psychosis - happen in 5% to 18% of people on high-dose regimens. These aren’t just "feeling off." They’re full psychotic episodes: hearing voices, believing things that aren’t true, acting strangely, or becoming completely withdrawn. Some patients don’t even realize they’re ill. That’s why family members often notice first.
When Do Symptoms Start?
Symptoms don’t wait months to show up. Most people begin noticing changes within the first few days. The median time to onset? Just three to four days after starting treatment. Some feel euphoric, overly confident, or unusually energetic. Others get agitated, confused, or anxious. Insomnia is one of the earliest red flags - trouble sleeping even when exhausted. By day five, confusion, irritability, or sudden personality shifts should raise concern.
And here’s something many don’t know: symptoms can appear even after you stop taking the drug. Case reports show psychosis and mania lasting weeks after the last pill. That means you can’t just assume everything’s fine once you taper off.
Who’s Most at Risk?
It’s not random. Certain people are far more likely to develop these problems:
- Women - Studies consistently show higher rates of psychiatric side effects in women, especially postmenopausal women.
- People over 65 - Aging brains are more sensitive to steroid effects on neurotransmitters and memory centers.
- Those with a history of depression, bipolar disorder, or prior psychosis - Even if it was years ago, past mental illness dramatically increases risk.
- People on high or long-term doses - The longer you’re on steroids and the higher the dose, the greater the chance of brain changes.
One study found that 1 in 6 patients on steroids developed mania with no depression at all. Another 1 in 4 had psychosis without any mood swings. That means you can’t just look for depression - you need to watch for anything unusual in behavior or thinking.

What’s Happening in the Brain?
Scientists aren’t 100% sure why this happens, but they’ve identified several key mechanisms. Corticosteroids flood the brain with cortisol-like chemicals, which can:
- Suppress the HPA axis - the body’s natural stress-response system - leading to imbalance in brain chemistry.
- Damage the hippocampus - the area responsible for memory and emotional regulation - reducing its ability to control fear and anxiety.
- Boost dopamine levels - in animal studies, steroids increased tyrosine hydroxylase, an enzyme that makes dopamine. Too much dopamine is strongly linked to psychosis.
These effects explain why memory problems are so common. Many patients report trouble remembering names, conversations, or even what day it is. It’s not just forgetfulness - it’s a real cognitive impairment tied directly to the drug.
What Does It Look Like in Real Life?
Here’s what this looks like outside textbooks:
- A 72-year-old woman with COPD starts on 60 mg of prednisone. Within five days, she stops recognizing her daughter, accuses her of stealing money, and refuses to eat because she thinks the food is poisoned.
- A 58-year-old man with rheumatoid arthritis becomes hyperactive, sleeps only two hours a night, spends all his savings on online gambling, and talks nonstop about becoming a millionaire.
- A 45-year-old woman develops severe insomnia, then begins hearing her dead mother calling her name. She doesn’t tell anyone because she thinks she’s "just stressed."
In all these cases, the symptoms started suddenly, didn’t match the person’s usual personality, and weren’t explained by any other illness. Once steroids were lowered or stopped, most improved - but not always quickly.
How Do Doctors Diagnose It?
There’s no blood test. No scan. Diagnosis is based on timing and exclusion. The DSM-5 criteria say steroid-induced psychosis must:
- Appear during or shortly after steroid use
- Include clear psychotic symptoms (delusions, hallucinations, disorganized speech)
- Not be better explained by another mental illness, drug use, infection, or metabolic issue
That means doctors must rule out everything else first - thyroid problems, brain tumors, infections like meningitis, alcohol withdrawal, or even vitamin B12 deficiency. Many patients get misdiagnosed with schizophrenia or bipolar disorder when it’s really the steroids.
That’s why experts stress: if someone on steroids suddenly acts out of character, assume it’s the drug until proven otherwise.
What’s the Treatment?
The first and most effective step? Reduce the dose. If possible, lower steroids to under 40 mg of prednisone per day - or even stop them entirely. About 92% of patients see full symptom relief once the dose is lowered.
But sometimes you can’t stop the steroids. A transplant patient, for example, needs them to survive. In those cases, doctors turn to off-label antipsychotics:
- Haloperidol - 0.5 to 1 mg per day
- Olanzapine - 2.5 to 20 mg per day
- Risperidone - 1 to 4 mg per day
These aren’t FDA-approved for this use, but multiple case reports show symptom improvement within days. Lithium has also been used to prevent mania, but it’s risky - kidney and thyroid damage, tremors, and toxicity make it a last-resort option.
Always involve a psychiatrist. This isn’t something to manage alone. A team approach - between your rheumatologist, pulmonologist, and mental health specialist - is critical.
What Should Patients and Families Do?
If you’re prescribed steroids, here’s what to do:
- Ask your doctor: "What are the mental side effects?" Don’t assume they’ll bring it up.
- Keep a daily log: Note sleep, mood, energy, and any strange thoughts or behaviors.
- Tell a family member to watch for changes - confusion, paranoia, aggression, or sudden euphoria.
- If symptoms start, don’t wait. Call your doctor immediately. Don’t try to tough it out.
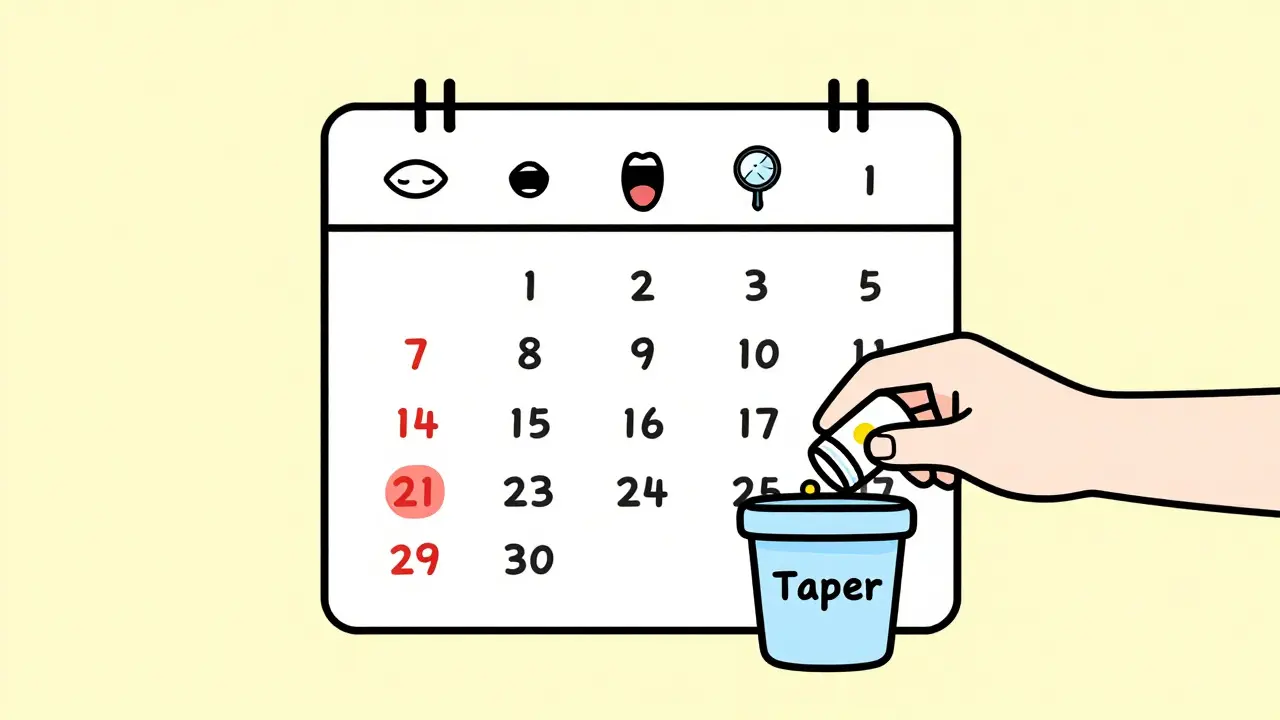
- Never stop steroids cold turkey. Tapering must be done under medical supervision.
Pharmacists can help too. Ask them for a printed list of side effects - many don’t even mention psychiatric risks on the label.
Why Isn’t This Better Known?
It’s shocking how little attention this gets. The FDA doesn’t require drug labels to highlight psychosis risk clearly. Medical guidelines are vague. Many doctors think "mood changes" mean just being irritable - not full psychosis. And because steroids are so widely used and often lifesaving, the focus stays on physical benefits.
But the cost of missing this is high. Patients lose jobs, relationships, and sometimes their freedom. Some end up in psychiatric hospitals. Others die by suicide. In one case, a man on steroids jumped from a bridge - he believed he was being watched by aliens. He had no prior mental illness. The steroids caused it.
Research is still catching up. We need better tools to detect early signs. We need biomarkers. We need clinical trials. Right now, we’re flying blind.
Bottom Line
Corticosteroids save lives. But they can also break minds. The risk of psychosis isn’t theoretical - it’s documented, predictable, and preventable. If you’re taking steroids, know the signs. If you’re caring for someone who is, watch closely. Early action can mean the difference between a temporary setback and a lifelong crisis.
There’s no magic pill to fix steroid-induced psychosis - but there is a simple one: awareness. Talk about it. Ask questions. Don’t let silence cost someone their sanity.



Zoe Brooks
January 18, 2026 AT 20:00Aysha Siera
January 20, 2026 AT 09:02Eric Gebeke
January 22, 2026 AT 08:35Joni O
January 23, 2026 AT 10:44Max Sinclair
January 25, 2026 AT 09:01Nishant Sonuley
January 25, 2026 AT 10:50Emma #########
January 26, 2026 AT 22:11Andrew McLarren
January 27, 2026 AT 18:53Andrew Short
January 27, 2026 AT 21:37Chuck Dickson
January 29, 2026 AT 15:02Robert Cassidy
January 29, 2026 AT 15:16Dayanara Villafuerte
January 29, 2026 AT 15:36Andrew Qu
January 30, 2026 AT 20:28