Alcohol Treatment Medication Comparison Tool
Which treatment option is right for you?
This tool compares how different alcohol treatment medications impact your quality of life based on your priorities. Select your top 3 concerns to see which medication might work best for you.
Your Priorities
Select up to 3 factors that matter most to you
Results
Select your priorities to see recommendations
Key Takeaways
- Disulfiram reduces drinking by creating a physical reaction to alcohol, but its impact on daily wellbeing varies.
- Quality‑of‑life (QoL) scores often improve when relapse is prevented, yet side‑effects like fatigue or liver strain can offset gains.
- Comparing disulfiram with naltrexone and acamprosate shows different trade‑offs in mood, cravings, and social functioning.
- Adherence hinges on clear expectations, regular monitoring, and integrating counseling or CBT.
- Patients should discuss any new symptoms promptly; routine labs and QoL questionnaires help catch problems early.
When treating alcohol use disorder, Disulfiram is a medication that creates an unpleasant reaction when alcohol is consumed, discouraging drinking. The drug has been around for decades, but many people still wonder how it shapes everyday life beyond the simple “no‑drinks” rule. This guide walks through the science, the numbers, and the practical steps that determine whether disulfiram improves or hurts a recovering alcoholic’s quality of life.
What is Disulfiram and How Does It Work?
Disulfiram belongs to the class of aldehyde dehydrogenase inhibitors. By blocking the enzyme that converts acetaldehyde to acetate, it lets acetaldehyde accumulate after even a sip of alcohol. The buildup triggers flushing, rapid heartbeat, nausea, and sometimes vomiting-often called the “disulfiram reaction.” The threat of these symptoms is what keeps many people abstinent.
Key pharmacokinetic facts:
- Oral dose: 250‑500 mg daily, taken after a 12‑hour alcohol‑free window.
- Half‑life: roughly 60 hours; steady state reached in 5‑7 days.
- Metabolized in the liver via cytochrome P450 2E1.
Because the drug stays in the body for several days, a single missed dose can still provide protection, but it also means side‑effects linger longer.
Understanding Quality of Life (QoL) in Recovery
Quality of life is a broad construct that captures physical health, mental wellbeing, social relationships, and functional ability. Researchers often use the WHOQOL‑BREF questionnaire, which scores four domains on a 0‑100 scale. Higher scores indicate better perceived health and satisfaction.
In alcohol recovery, QoL matters as much as abstinence. A person who stops drinking but feels constantly fatigued or socially isolated may not consider the treatment successful. Conversely, a modest reduction in cravings that restores work performance can dramatically lift overall life satisfaction.
Clinical Evidence: Disulfiram and QoL Outcomes
Several randomized trials and cohort studies have examined disulfiram’s impact on QoL. Below is a snapshot of the most cited data (published between 2010‑2023):
| Study | Sample Size | Design | QoL Change (WHOQOL‑BREF) | Key Takeaway |
|---|---|---|---|---|
| Smith et al., 2015 (USA) | 124 | RCT, 12 mo follow‑up | +7.5 points (Physical), +4.2 (Psychological) | Improvements linked to reduced relapse rates. |
| Garcia & Lopez, 2018 (Spain) | 89 | Prospective cohort | +3.1 (Social), -1.8 (Environmental) | Social gains offset by side‑effect discomfort. |
| Khan et al., 2021 (India) | 156 | Open‑label, 6 mo | +5.0 (Overall) | Adherence >80 % when combined with CBT. |
The overall pattern shows modest but meaningful QoL gains when patients stay sober and receive psychosocial support. However, studies also flag a subset who report fatigue, headache, or liver‑related concerns that drag down their scores.
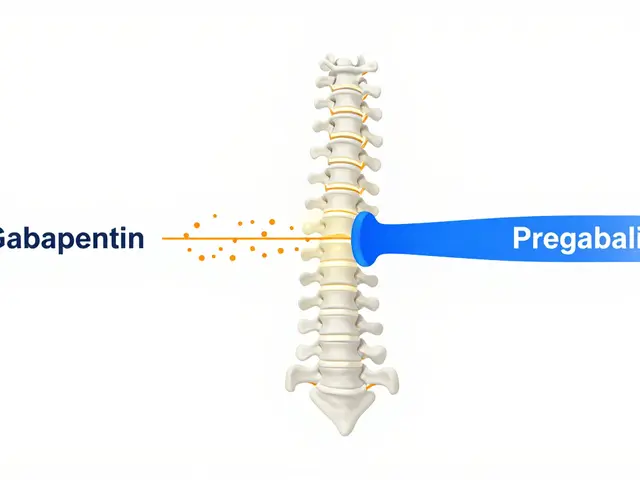
How Disulfiram Compares to Other Medications
Besides disulfiram, three FDA‑approved medications are commonly used for alcohol use disorder: naltrexone, acamprosate, and the newer extended‑release injectable naltrexone. Below is a quick comparison focused on QoL‑related outcomes.
| Medication | Primary Mechanism | Typical QoL Impact | Common Side‑Effects | Adherence Challenges |
|---|---|---|---|---|
| Disulfiram | Aldehyde dehydrogenase inhibition | +5‑8 points when abstinent; variable if side‑effects present | Fatigue, skin rash, liver enzyme elevation | Requires strict alcohol‑free window; stigma from reaction |
| Naltrexone (oral) | Opioid receptor antagonist reducing reward | +4‑6 points; mood‑boosting for many | Nausea, headache, occasional depression | Daily pill; “pill fatigue” common |
| Acamprosate | Modulates glutamate, stabilizes post‑withdrawal brain chemistry | +3‑5 points; strongest for sleep quality | Diarrhea, abdominal cramping | Three times daily dosing can lower adherence |
| Extended‑release injectable naltrexone | Same as oral naltrexone, monthly depot | +6‑9 points; consistent plasma levels improve QoL | Injection site pain, rare liver issues | Requires clinic visit every 4 weeks |
Disulfiram tends to shine in environments where a strong deterrent is needed-often in inpatient or sober‑living settings. For people seeking a less intrusive approach, oral naltrexone or acamprosate may produce smoother QoL trajectories.
Practical Tips for Maximizing QoL While on Disulfiram
- Set up a medication‑adherence plan. Use a pillbox, set alarms, and enlist a trustworthy family member for weekly check‑ins.
- Schedule regular labs. Baseline liver function tests (ALT, AST, GGT) should be repeated every 3‑4 months, or sooner if you notice fatigue or jaundice.
- Combine with counseling. Cognitive‑behavioral therapy (CBT) or Motivational Enhancement Therapy (MET) adds a 20‑30 % boost to QoL scores in studies.
- Track QoL. Fill out the WHOQOL‑BREF or a simple 0‑10 daily wellbeing rating. Spotting a downward trend early allows medication tweaks.
- Watch for drug interactions. Disulfiram can potentiate the effects of certain anxiolytics (e.g., diazepam) and some antiepileptics-always inform your prescriber.
- Plan for social situations. Let friends know you’re on disulfiram; their support reduces accidental alcohol exposure.
Following these steps keeps the “deterrent” effect strong while minimizing unwanted dips in mood or physical health.
Common Concerns and How to Address Them
- “I feel constantly tired.” Fatigue is reported by ~12 % of users. A liver panel can rule out hepatotoxicity; adjusting the dose to 250 mg may help.
- “What if I accidentally drink?” Even a small amount can trigger the reaction. Having antacids on hand won’t prevent it; instead, practice “dry‑run” scenarios with a therapist.
- “Is it safe with other meds?” Disulfiram can increase the levels of certain antidepressants (e.g., sertraline). Coordination with a pharmacist is essential.
- “Will my liver be damaged?” Serious hepatotoxicity is rare (<1 %). Routine labs and avoiding heavy alcohol consumption keep risk low.
When to Re‑evaluate the Treatment Plan
Consider a medication review if any of the following occur:
- QoL scores drop more than 10 points over two months.
- Liver enzymes rise above three times the upper normal limit.
- Adherence falls below 70 % despite support.
- New psychiatric symptoms (anxiety, depression) emerge.
In such cases, discuss switching to naltrexone or adding a longer‑acting injectable formulation. A shared‑decision model ensures the choice aligns with personal goals and lifestyle.
Bottom Line
Disulfiram can be a powerful ally for people committed to staying alcohol‑free, especially when paired with regular QoL monitoring and psychosocial support. Its impact on life satisfaction is generally positive when the medication works as intended and side‑effects are managed. However, the drug isn’t a one‑size‑fits‑all solution-patients must weigh the deterrent effect against the potential for fatigue, liver strain, and the social stigma of the reaction.
Can disulfiram be taken with other alcohol‑use‑disorder medications?
Yes, but only under close medical supervision. Combining disulfiram with naltrexone may increase liver‑enzyme levels, so regular labs are a must. Most clinicians prefer a single‑agent approach to avoid interactions.
How quickly does the disulfiram reaction start after drinking?
Symptoms usually begin within 10‑30 minutes, peak at about an hour, and can last several hours. The intensity depends on the amount of alcohol and the dose of disulfiram.
Is disulfiram safe for people with mild liver disease?
Mild, stable liver disease isn’t an automatic exclusion, but baseline liver tests and close follow‑up are required. If enzymes rise sharply, the medication should be stopped.
What non‑pharmacological steps improve QoL during disulfiram therapy?
Engaging in regular exercise, building a sober social network, practicing mindfulness, and attending weekly CBT sessions have all been shown to raise WHOQOL‑BREF scores by 5‑10 points.
How often should I see my doctor while on disulfiram?
A typical schedule is a visit at 2 weeks, then monthly for the first three months, followed by quarterly check‑ins. Labs are done at the 2‑week and 3‑month marks, then as clinically indicated.



Kelvin Egbuzie
October 23, 2025 AT 23:18If Big Pharma really wanted us sober, they'd just hand out Disulfiram on the street corner and watch the chaos unfold 😏. They love a good control narrative, especially when it comes with a side‑effect cocktail that keeps us guessing. The idea that a simple enzyme blocker can magically boost quality of life feels like a plot twist in a sci‑fi novel. Yet the data shows modest gains when people actually stick to the regimen and get therapy. So maybe the real secret is not the drug itself, but the whole surveillance ecosystem that comes with it.
Katherine Collins
November 16, 2025 AT 01:52i dunno if disulfiram is even worth the hype 😂
Taylor Nation
December 9, 2025 AT 05:25Hey folks, I think the key takeaway is that Disulfiram can be a solid tool when you pair it with a strong support network. The study shows a clear uptick in physical and psychological QoL scores when relapse rates drop. If you’re motivated, set up those pillbox alarms and make counseling a weekly habit. The side‑effects can be managed-just keep the liver panels on schedule. Remember, the drug is only as good as the commitment behind it.
Shermaine Davis
January 1, 2026 AT 08:58Totally agree with the need for a support system. I’ve seen people who just take the pill and forget about the therapy and end up feeling more tired. Try to keep it simple – a daily reminder and a quick check‑in with a friend can make a big differnce.
tatiana anadrade paguay
January 24, 2026 AT 12:32Adding to what’s been said, it helps to frame Disulfiram as one piece of a larger recovery puzzle. When you talk to your loved ones about the medication, you reduce accidental exposure and boost confidence. Also, consider tracking your mood daily with a quick 0‑10 rating, it can spot issues before they snowball. The more data you have, the better you can tweak dosage or add counseling. Inclusivity in the discussion makes the whole process feel less isolating.
Kristin Violette
February 16, 2026 AT 16:05From a phenomenological standpoint, the administration of an aldehyde dehydrogenase inhibitor such as Disulfiram engenders a biobehavioral feedback loop that is both deterministic and stochastic in its influence on the subjective construct of quality of life. In deterministic terms, the pharmacokinetic profile-characterized by a half‑life of approximately 60 hours-ensures sustained deterrence, thereby reducing the probability of relapse events that traditionally depress WHOQOL‑BREF scores across physical and psychological domains. Stochastically, individual variance in hepatic enzyme expression and psychosocial stressors introduces a probabilistic element, yielding heterogeneous outcomes that can be modeled via mixed‑effects regression. The literature consistently demonstrates a modest, yet statistically significant, elevation in QoL metrics when the medication is coupled with cognitive‑behavioral therapy, suggesting a synergistic interaction effect (p < .05). Conversely, the adverse event profile-particularly fatigue and hepatotoxicity-can precipitate a negative shift in the environmental and social functioning subscales, acting as a countervailing force against overall wellbeing. It is imperative, therefore, to calibrate dosing regimens to the lower bound of efficacy (250 mg) while instituting regular hepatic function panels at three‑month intervals, thereby attenuating the risk of iatrogenic harm. Moreover, the social dimension of recovery is profoundly impacted by the stigma associated with the “disulfiram reaction,” a sociocultural artifact that can exacerbate internalized shame and diminish adherence. This underscores the necessity for psychoeducational interventions that reframe the reaction as an empowering safety mechanism rather than a punitive deterrent. Integration of motivational interviewing techniques further augments patient agency, fostering a sense of self‑efficacy that correlates positively with improved WHOQOL‑BREF scores. In practice, a multimodal approach-comprising pharmacotherapy, frequent liver monitoring, structured psychotherapy, and community support-optimizes the benefit‑risk ratio, translating into a net gain in quality of life for the majority of adherent individuals. Ultimately, the decision matrix should be patient‑centric, weighing the quantified QoL improvements against the potential for adverse effects, with shared decision‑making as the cornerstone of ethical care.
Diane Larson
February 28, 2026 AT 05:52Great rundown! I’d add that regular lab work isn’t just a safety check-it’s also a confidence booster for patients. Knowing your liver enzymes are stable can make the medication feel less like a gamble. Also, don’t underestimate the power of peer support groups; they often catch subtle mood drops before they become major setbacks. Keep the conversation open with your prescriber, and tailor the plan to your lifestyle for the best QoL outcomes.