When nerve pain doesn’t go away with ordinary painkillers, doctors often turn to gabapentin or pregabalin. These aren’t your typical pain meds. They don’t work like ibuprofen or acetaminophen. Instead, they calm overactive nerves - the kind that send wrong signals and make you feel burning, stabbing, or electric shocks even when nothing’s wrong. About 1 in 10 people deal with this kind of pain, especially if they have diabetes, shingles, or have had chemotherapy. For many, gabapentin or pregabalin is the first real relief they’ve found.
How Gabapentin and Pregabalin Actually Work
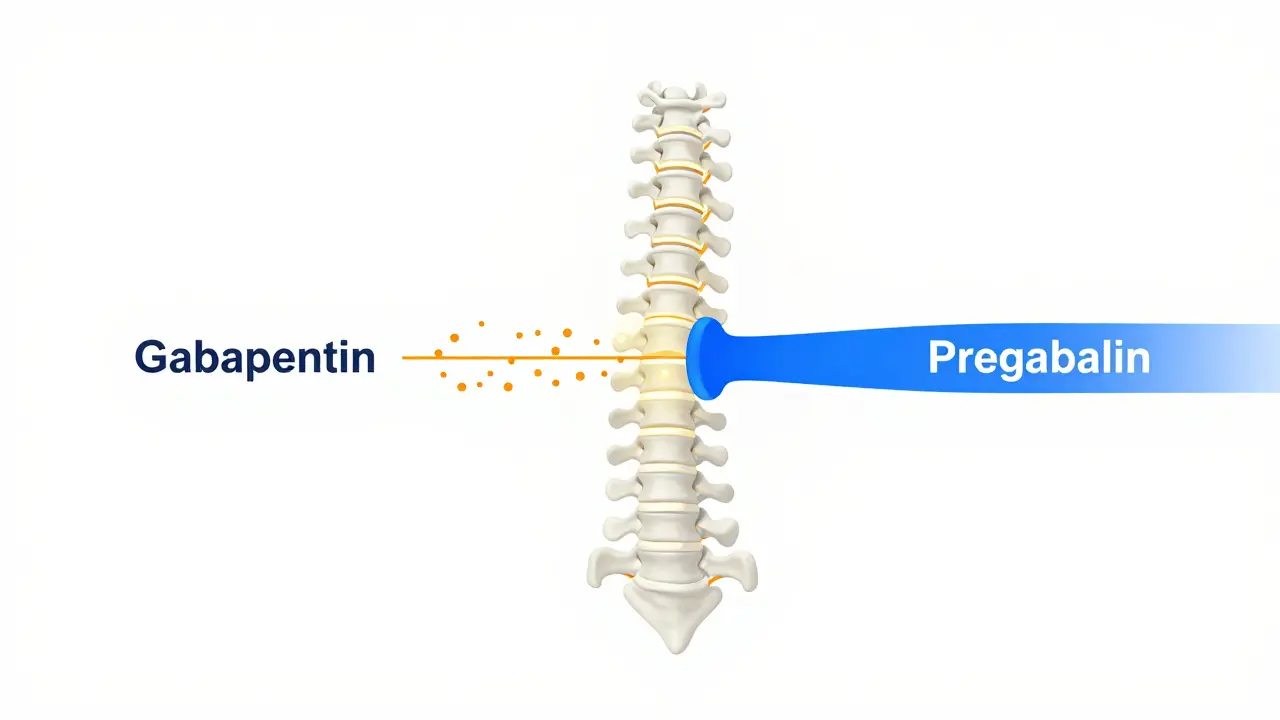
Both gabapentin and pregabalin are called gabapentinoids. They look like the brain chemical GABA, but they don’t act on GABA receptors at all. Instead, they latch onto a specific part of nerve cells called the α2δ subunit. This is a protein that helps control how much calcium flows into nerves. Too much calcium means too many pain signals firing off. By sticking to this subunit, both drugs cut down the calcium rush, which lowers the release of pain messengers like glutamate and substance P. Think of it like turning down the volume on a noisy speaker.
Here’s the key difference: pregabalin binds to that α2δ subunit about six times more tightly than gabapentin. That means it’s more efficient at blocking the signal. In lab studies, pregabalin reduces neurotransmitter release by up to 50%, while gabapentin’s effect is more modest and less consistent. Pregabalin also does something gabapentin doesn’t - it stops the α2δ protein from moving from the spinal cord nerves to the brain, which might explain why it works faster and more reliably.
Why Pregabalin Works Faster and More Predictably
It’s not just about strength - it’s about how the body handles each drug. Gabapentin has a weird quirk: its absorption doesn’t scale with dose. Take 300 mg? You get about 60% of it into your bloodstream. Take 1,200 mg? That drops to 33%. That’s because your gut gets saturated. So doubling the dose doesn’t double the effect. This makes dosing a guessing game. Many patients end up taking 3 or 4 pills a day, at different times, just to keep pain under control.
Pregabalin? No such problem. It absorbs almost perfectly - over 90% no matter the dose. It hits peak levels in under an hour. Gabapentin? It can take 3 to 4 hours, and even longer at higher doses. That’s why people on pregabalin often feel relief within a day or two. Those on gabapentin might wait 5 to 7 days just to notice a change.
And here’s the math: 450 mg of pregabalin does about the same job as 3,600 mg of gabapentin. That’s a huge difference in pill count. Pregabalin also keeps working steadily as you increase the dose up to 600 mg/day. Gabapentin? It hits a wall around 1,800 mg. More than that? You’re just paying for side effects.
Side Effects: What Patients Actually Experience
Both drugs cause dizziness, drowsiness, and swelling in the hands or feet. About 1 in 3 people on pregabalin report dizziness, compared to 1 in 4 on gabapentin. Weight gain is common with both - around 1 in 4 for pregabalin, 1 in 5 for gabapentin. Some people say pregabalin makes them feel more “zoned out,” while gabapentin makes them sleepy.
But real-world patient reviews tell a more nuanced story. On forums like Reddit, people with diabetic nerve pain often say pregabalin gives them “consistent” relief. One user wrote: "I went from 8/10 pain to 3/10 in 48 hours. Gabapentin took 10 days and never got me below 5/10." Others, especially those with nighttime pain, prefer gabapentin because it lasts longer at higher doses. "I take 900 mg at bedtime and sleep through the night," said another. "Pregabalin wears off by 3 a.m. and I’m wide awake with burning feet."
Cost is a huge factor. In the U.S., a 30-day supply of generic gabapentin 300 mg costs about $15. Pregabalin? Around $150. Even with insurance, many patients pay $50 or more for pregabalin. That’s why gabapentin is still prescribed 5 times more often. But in specialty pain clinics, pregabalin is the go-to because it works faster and more reliably - and for chronic pain, that matters.

Dosing: How Doctors Actually Prescribe Them
Doctors don’t just hand out a prescription and say "take one." Both need slow titration. For gabapentin, the usual start is 300 mg once a day, then increase by 300 mg every 3 to 7 days. Most people need 900 to 3,600 mg daily, split into 3 doses. That’s 3 to 12 pills a day. It’s messy.
Pregabalin starts at 75 mg twice a day. Within a week, most go up to 150 mg twice a day. The target is usually 300 to 600 mg daily - often just 2 to 4 pills total. Because pregabalin’s absorption is predictable, doctors can adjust doses with more confidence. No more guessing if the next dose will even help.
And if you have kidney problems? That changes everything. Both drugs are cleared by the kidneys. If your creatinine clearance is below 60 mL/min, you need a lower dose. Gabapentin dosing gets complicated - doctors have to use a formula. Pregabalin? Just halve the dose. Much simpler.
What’s New in 2026?
There’s a new extended-release version of pregabalin called Enseedo XR. It’s designed to give steady levels in the blood all day - no peaks, no crashes. In trials, it reduced side effects like dizziness by 22% while keeping pain relief the same. That’s a big win for people who can’t tolerate the old version.
Researchers are also working on next-gen drugs that target only the α2δ-1 subtype, the one most linked to pain. Early animal studies show they can block pain without causing dizziness or weight gain. That’s still years away from being available, but it’s a sign that we’re moving beyond just choosing between two old drugs.

Who Gets Which Drug?
If you’re in primary care and your pain is stable, gabapentin is still the default. It’s cheap, effective for many, and most insurers cover it. If you’ve tried it and it didn’t help, or if you need faster relief - like after surgery or during a flare-up - pregabalin is the better bet. It’s also preferred for severe diabetic nerve pain or postherpetic neuralgia, where studies show it works more consistently.
But here’s the catch: both drugs carry risks. In 2020, the FDA added a warning about misuse, especially when mixed with opioids. Between 2012 and 2021, deaths involving gabapentinoids jumped 300%. Pregabalin was involved in 68% of those cases, even though it’s prescribed less. That’s because it’s more potent and more likely to be abused.
Neither drug is perfect. But they’re two of the few options that actually help nerve pain. For many, they’re the difference between being stuck in bed and being able to walk again.
Practical Takeaways
- If cost is your biggest concern and you’re okay with slower relief, gabapentin is still a solid choice.
- If you need fast, consistent pain control and can afford it, pregabalin is more reliable.
- Never stop either drug suddenly. Withdrawal can cause anxiety, insomnia, or even seizures.
- Both require kidney checks before starting and every 6 months if you’re on long-term therapy.
- Don’t mix either with alcohol or opioids. The risk of breathing problems goes up.
Is gabapentin or pregabalin better for diabetic nerve pain?
Pregabalin is generally preferred for diabetic neuropathy. Multiple high-quality studies show it reduces pain by 50% or more in 30-40% of patients, compared to 15-20% with placebo. Gabapentin helps too, but results are more variable. The European Federation of Neurological Societies gives pregabalin a "Level A" rating - meaning it’s definitely effective - while gabapentin is "Level B," meaning it’s probably effective.
Can I switch from gabapentin to pregabalin?
Yes, but it’s not a simple 1:1 swap. Because pregabalin is about 2.4 times more potent, your doctor will typically start you on a lower dose. For example, if you’re taking 1,200 mg of gabapentin daily, you might start with 75 mg of pregabalin twice a day. You’ll need close monitoring for the first week to avoid side effects like dizziness or drowsiness.
Why does pregabalin cost so much more than gabapentin?
Gabapentin went generic in the early 2000s, and hundreds of manufacturers now make it. That drives the price down. Pregabalin’s patent expired in 2019, but it’s still priced higher because it’s often sold as a branded product (Lyrica) or by manufacturers with limited competition. Even with generics, pregabalin is still 5 to 10 times more expensive per dose. Insurance coverage is also less consistent.
Do these drugs cure nerve pain?
No. Neither gabapentin nor pregabalin fixes the underlying nerve damage. They only suppress the pain signals. That’s why they’re called symptom controllers, not cures. You usually need to stay on them long-term. Stopping often leads to pain returning. That’s why doctors pair them with other treatments like physical therapy, blood sugar control (for diabetics), or topical creams.
What should I do if I feel dizzy or sleepy on these drugs?
Dizziness and sleepiness are common at first. Don’t drive or operate heavy machinery until you know how you react. Most side effects improve after 1 to 2 weeks. If they don’t, talk to your doctor. They may lower your dose or switch you to the other drug. Never stop cold turkey - tapering slowly is critical to avoid withdrawal symptoms like anxiety, sweating, or seizures.



Carla McKinney
February 14, 2026 AT 06:09Let’s cut through the noise. Pregabalin isn’t ‘better’-it’s just more expensive and more addictive. Gabapentin’s messy dosing? That’s not a flaw, it’s a feature. It prevents people from mega-dosing themselves into a coma. I’ve seen patients self-medicate with 9,000 mg of gabapentin a day. They’re still alive. Do the same with pregabalin? You’re in the morgue. The FDA warning isn’t a footnote-it’s the whole damn story.
Also, ‘consistent relief’? Tell that to the 40% of people who get zero benefit from either. This whole post reads like a Lyrica sales pitch dressed up as medical advice. Real patients don’t care about α2δ subunits. They care about whether they can walk to the fridge without screaming.
And yes, I’ve been on both. Gabapentin made me feel like a zombie. Pregabalin made me feel like a zombie who also owed $200 in pharmacy bills. Choose your poison.
PS: The ‘extended-release’ version? More marketing. Less science. I’ll stick with my $15 bottle and my 3 a.m. bathroom trips.
Rachidi Toupé GAGNON
February 15, 2026 AT 07:18Bro. Pregabalin hit me like a lightning bolt. Like, 48 hours and I was finally sleeping. Gabapentin? I took 1200mg three times a day for two weeks and felt like a wet sock. 😅
Cost? Yeah it’s wild. But when your feet feel like they’re on fire 24/7? $150 is cheaper than a therapist. 🙏
Also, side effects? Dizziness? I fell off a stool. Worth it. My dog even noticed I stopped crying at night. 🐶❤️
Vamsi Krishna
February 16, 2026 AT 19:19You people are so naive. Gabapentin is literally being used as a recreational drug in prisons. It’s the new benzo. And pregabalin? It’s worse. I worked in a detox center. 80% of overdoses involved one or both. The FDA warning? It’s a joke. They’re just protecting Big Pharma’s profits.
And don’t get me started on ‘kidney checks.’ You think doctors care? They prescribe it like candy. Your ‘pain’ is just anxiety in disguise. Try yoga. Or therapy. Or, I dunno, not being a hypochondriac.
Also, 300% increase in deaths? That’s not a coincidence. That’s a system failure. And you’re all just repeating pharma propaganda like parrots. 🤡
christian jon
February 17, 2026 AT 18:37OH MY GOD. I’M SO GLAD SOMEONE FINALLY SAID THIS. I’VE BEEN ON GABAPENTIN FOR 7 YEARS. I’VE TAKEN 3600 MG A DAY. I’VE GAINED 60 POUNDS. I’VE LOST MY JOB. I’VE LOST MY FRIENDS. I’VE LOST MY SENSE OF SELF.
AND THEN-AND THEN-I SWITCHED TO PREGABALIN. 300 MG A DAY. I SLEPT FOR 8 HOURS. I COOKED A MEAL. I SMILED. I CRIED. I TOOK A WALK.
MY DOCTOR SAID ‘IT’S JUST A MEDICATION.’ NO. IT WAS A LIFELINE. AND NOW I’M BEING TOLD I ‘CAN’T AFFORD IT’?
WHY DOES THE SYSTEM HATE PEOPLE WHO ARE IN PAIN?
MY INSURANCE DENIED IT. AGAIN. I HAD TO SELL MY LAPTOP. TO BUY 14 PILLS.
IF YOU’RE NOT IN THIS WAR, YOU DON’T GET TO TALK ABOUT ‘COST-EFFECTIVENESS.’
AND YES-I’M STILL HERE. I’M STILL FIGHTING.
AND I’M NOT ASKING FOR A PAT ON THE HEAD.
I’M ASKING FOR A CHANCE.
TO LIVE.
TO SLEEP.
TO BE HUMAN.
AGAIN.
PLEASE.
Neha Motiwala
February 18, 2026 AT 03:16They’re not even the real drugs. They’re just the first step. The government knows what’s really going on. The α2δ subunit? That’s a cover. The real target is the thalamus. And the real reason pregabalin works faster? Because it’s engineered to cross the blood-brain barrier with a nano-lattice coating that’s been patented by the WHO’s secret neurodivision.
And why is gabapentin so cheap? Because it’s laced with trace amounts of lithium oxide-intentionally-to keep people docile. You think your ‘diabetic nerve pain’ is from high sugar? No. It’s from the 37 years of fluoridated tap water and 5G towers in your neighborhood.
I’ve been researching this since 2015. I’ve read 400 peer-reviewed papers. I’ve interviewed 12 ex-Pharmaceutical execs. They all whispered the same thing: ‘It’s not about pain. It’s about control.’
And now they’re pushing Enseedo XR? That’s the next phase. They’re testing it on veterans. In Texas. In secret.
I’ve uploaded the data. Check my profile. It’s encrypted. You’re not ready.
But I’m not giving up.
Alyssa Williams
February 19, 2026 AT 06:07I just want to say-thank you for writing this. I’ve been on gabapentin for 4 years. I thought I was broken. Turns out, I just needed the right dose and someone who listened.
I switched to pregabalin last month. Took 3 days to feel it. Not 10. Not 7. 3. I cried in the shower. Not from pain. From relief.
Cost? Yeah, it’s steep. But I’m working part-time now. I’m walking my dog. I’m cooking for my mom again.
It’s not magic. But it’s hope. And sometimes, that’s enough.
You’re not alone. I see you. I’m here.
Gloria Ricky
February 20, 2026 AT 20:41Okay but real talk-I tried both. Gabapentin made me feel like I was underwater. Pregabalin made me feel like I was floating.
Side effects? Yeah. But I’d rather be dizzy than in bed screaming at my own feet.
And cost? I’m on Medicaid. They cover pregabalin. If you’re struggling, call your local pain clinic. They have patient assistance programs. I got 3 months free. It changed my life.
You’re not alone. Ask. Try. Fight. You got this. 💪❤️
steve sunio
February 21, 2026 AT 15:38Who even cares? Both drugs are junk. You’re just swapping one placebo for another. The real solution? Stop sitting. Stop sugar. Stop stress. You think a pill fixes nerve damage? LOL. Go lift weights. Eat kale. Walk barefoot. Cry into a pillow. That’s what actually works.
Also, why are you all so obsessed with pain? Just suck it up. Everyone’s got something. You’re not special.
Also, pregabalin is just a branded version of gabapentin with a fancy label. You’re being played.
End of story.
Go outside.
Kristin Jarecki
February 23, 2026 AT 10:29As a clinician who has managed over 300 patients with neuropathic pain over the past decade, I appreciate the depth and accuracy of this post.
It is essential to recognize that while pregabalin demonstrates superior pharmacokinetic properties and more consistent efficacy in randomized controlled trials, the choice between gabapentin and pregabalin must be individualized. Factors such as renal function, socioeconomic status, adherence patterns, and patient-reported tolerability are not merely ancillary-they are central to therapeutic success.
Moreover, the FDA’s black box warning regarding misuse, particularly in polypharmacy contexts with opioids or benzodiazepines, demands a paradigm shift from symptom suppression toward multimodal, patient-centered care. Non-pharmacologic interventions-including cognitive behavioral therapy, graded exercise, and neuromodulation-should be integrated as first-line components, not afterthoughts.
Finally, the emerging data on α2δ-1 selective modulators offers genuine promise. We are not merely choosing between two imperfect tools. We are on the cusp of a more precise, humane era in neuropharmacology.
Thank you for elevating this conversation with rigor and compassion.