CGM Trend Arrow Insulin Calculator
Adjust insulin doses using Endocrine Society guidelines based on your CGM trend arrows. Enter your current blood sugar, correction factor, and the arrow pattern to get precise adjustment recommendations.
Enter values to see insulin adjustment recommendation
When your blood sugar is dropping fast and your CGM shows two downward arrows, should you skip your next insulin dose? What if it’s rising quickly before dinner-do you add more insulin, and by how much? For people using insulin or other diabetes medications, these aren’t just hypothetical questions. They’re daily decisions that can mean the difference between a safe day and a trip to the ER. Continuous Glucose Monitoring (CGM) doesn’t just show you your current number-it tells you where your glucose is headed. And when you learn how to read those trend arrows, you can stop reacting to highs and lows and start preventing them.
What CGM Trend Arrows Really Mean
Your CGM doesn’t just give you a number. It gives you direction. Most systems-like Dexcom G6, G7, and Abbott Libre 3-use arrows to show how fast your glucose is moving. There are five main arrow patterns:- Double-up (↑↑): Glucose is rising fast-more than 2 mg/dL per minute.
- Single-up (↑): Glucose is rising slowly-about 1 to 2 mg/dL per minute.
- Flat (→): Glucose is steady-no major change in the last 15-30 minutes.
- Single-down (↓): Glucose is falling slowly-about 1 to 2 mg/dL per minute.
- Double-down (↓↓): Glucose is falling fast-more than 2 mg/dL per minute.
Why Trend Arrows Beat Fingersticks
Traditional blood glucose meters only show you where you are right now. A reading of 140 mg/dL could mean you’re about to crash, or you’re about to climb. Without context, you’re guessing. CGM trend arrows remove that guesswork. A 2017 study in Diabetes Technology & Therapeutics found that people who adjusted insulin based on trend arrows had 28% fewer low blood sugar events and spent 17% more time in the target range (70-180 mg/dL) than those who relied only on fingersticks. Why? Because CGM lets you act before the problem happens. If you see a double-down arrow at 3 a.m., you can eat a small snack before your sugar hits 50. If you see a double-up before lunch, you can give a little extra insulin now instead of chasing a high later.How Much to Adjust: The Endocrine Society Rules
The Endocrine Society published clear, science-backed guidelines in 2017 for adjusting insulin doses using trend arrows. These aren’t suggestions-they’re standardized protocols used by endocrinologists across the U.S. and Europe. The key is your correction factor-how much one unit of insulin lowers your blood sugar. For example, if your correction factor is 1:50 (1 unit lowers glucose by 50 mg/dL), here’s what you do:- Double-up arrow: Add 1.2 units to your meal or correction dose.
- Single-up arrow: Add 0.8 units.
- Flat arrow: No change.
- Single-down arrow: Reduce by 0.8 units.
- Double-down arrow: Reduce by 1.2 units.

What About Non-Insulin Medications?
Most people think CGM is only for insulin users. But it’s just as important for those on SGLT2 inhibitors like empagliflozin (Jardiance) or dapagliflozin (Farxiga). These drugs lower blood sugar by making your kidneys flush out glucose. But they can also cause euglycemic diabetic ketoacidosis-a dangerous condition where your blood sugar stays normal, but your body starts burning fat for fuel because you’re low on insulin. The 2024 ADA/EASD consensus report recommends reducing SGLT2 inhibitor doses if your CGM shows persistent glucose under 180 mg/dL with ketones above 0.6 mmol/L. That’s a new use case. If your CGM shows steady lows or frequent dips-even if your numbers look fine-you might need to talk to your doctor about adjusting your medication, not just your insulin.Common Mistakes and How to Avoid Them
Even with clear rules, people still mess up. Here are the top three errors-and how to dodge them:- Stacking insulin: You give a correction dose for a high, then 30 minutes later see another high and give more-without checking if the first dose is still working. Result? A crash. Always check your insulin-on-board (IOB) before giving more. Most CGMs show this automatically.
- Overreacting to sensor lag: After exercise or a meal, your CGM might show a slow rise while your real blood sugar is already dropping. Don’t add insulin just because the arrow is up. Wait 10-15 minutes, check another reading, or do a fingerstick if you’re unsure.
- Ignoring context: A double-down arrow at 2 a.m. might mean you need a snack. But if you just took 2 units of insulin for a high at midnight, the arrow might be showing the effect of that dose-not a new trend. Always ask: What happened in the last hour?
Real People, Real Results
On Reddit’s r/typeonegrit, one user named InsulinWizard42 cut their weekly lows from 3.2 to 0.7 after using the Endocrine Society rules. They said: “The specific unit adjustments took the guesswork out of dosing when my sugar was trending up before meals.” But it’s not always smooth. A user on Diabetes Daily doubled their insulin for a double-up arrow and ended up with a 45 mg/dL low-because they didn’t check their IOB. That’s why education matters. A 2021 survey by Beyond Type 1 found that 68% of CGM users adjust doses using trend arrows, and 82% of them say it improved their time-in-range. But 32% didn’t use them at all-mostly because they were afraid of making a mistake or never got proper training.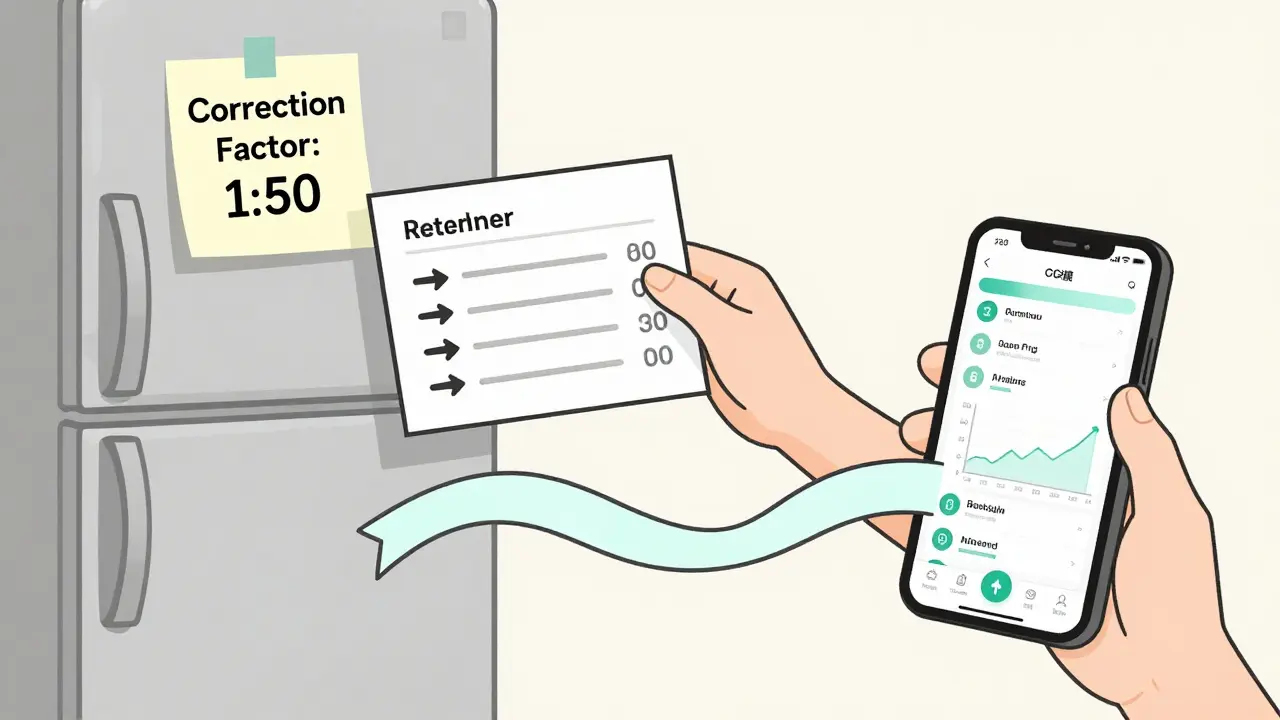
What You Need to Get Started
You don’t need to be a math genius. But you do need three things:- Your correction factor: Ask your doctor or diabetes educator. It’s usually calculated as 1800 divided by your total daily insulin dose (for rapid-acting insulin).
- A working CGM: Make sure your sensor is fresh (Dexcom sensors last 10 days, Libre 3 lasts 14). Old sensors give laggy data.
- One simple reference card: Print out the Endocrine Society adjustment table. Tape it to your fridge or save it in your phone. You don’t need to memorize it.
The Future: Apps That Do It For You
The FDA approved DAFNE+ in May 2023-the first app that automatically calculates insulin adjustments using your CGM trend arrows. It pulls your glucose data, correction factor, and insulin-on-board, then tells you exactly how much to give. In trials, it cut user errors by 62%. You don’t have to do the math anymore. But even with automation, you still need to understand what’s happening. If the app says “add 1.2 units,” you should know why. Otherwise, you’re trusting a machine without knowing the rules.Final Thought: CGM Is a Tool, Not a Crutch
CGM doesn’t replace knowledge-it enhances it. Trend arrows turn passive monitoring into active control. But they only work if you know how to use them. Don’t wait for a bad low or a scary high to learn. Start today. Check your arrows. Learn your correction factor. Talk to your care team. The goal isn’t perfect numbers-it’s fewer surprises, fewer hospital visits, and more days where you feel in charge of your diabetes.Can I adjust my insulin dose based on CGM trend arrows if I’m not on insulin?
No, trend arrow-based insulin adjustments only apply to people using insulin. However, CGM data can still help guide other medications. For example, if you’re on an SGLT2 inhibitor and your CGM shows persistent low glucose with ketones above 0.6 mmol/L, your doctor may recommend lowering your dose to prevent diabetic ketoacidosis-even if your blood sugar looks normal. Always consult your provider before changing any diabetes medication.
What if my CGM shows a double-down arrow but I just ate?
If you just ate and your glucose is falling fast, your insulin dose may have been too high, or your carbs were lower than you thought. Don’t reduce your insulin for the next meal just because of this one trend. Instead, check your blood sugar in 30 minutes. If it’s still dropping, have a small snack with 15 grams of fast-acting carbs. Next time, consider lowering your pre-meal insulin or increasing your carb estimate.
Do all CGM devices use the same trend arrows?
Most use similar symbols, but the speed thresholds vary. Dexcom defines a double-up arrow as a rise faster than 2 mg/dL per minute. Abbott’s Libre 3 uses 3 mg/dL per minute. Always check your device’s manual. The Endocrine Society guidelines were based on Dexcom data, but the principles apply across devices-just adjust the speed thresholds accordingly. If you switch CGMs, re-learn what each arrow means on your new device.
How long does it take to get good at using trend arrows?
Most people feel confident after 2-4 weeks of daily use. The first week is usually about learning your patterns-when your sugar rises after coffee, drops after walking, or spikes after stress. By week three, you’ll start noticing trends you didn’t see before. Don’t rush. Use the reference card. If you’re unsure, stick to your usual correction dose until you’re confident.
Can I rely on CGM trend arrows during exercise?
Exercise can cause misleading trends. A double-down arrow during a run might mean your glucose is dropping-but it could also mean your body is using glucose faster, not that you’re low. The same goes for a double-up after exercise-it might be a stress response, not a need for insulin. Use trend arrows as a guide, not a rule, during physical activity. Check your blood sugar before, during (if possible), and after. Many people reduce insulin or eat extra carbs before workouts based on past experience, not real-time arrows.




Dylan Smith
December 16, 2025 AT 13:47Finally someone explains this without jargon. I used to guess my doses until I started watching the arrows. Now I don’t wake up at 3am panicked. It’s like having a co-pilot for my blood sugar.
Also the 0.8 unit adjustments? Game changer.
Souhardya Paul
December 17, 2025 AT 10:56This is exactly what my endo tried to teach me but I was too overwhelmed to listen. I printed the table and taped it to my insulin pump. Now I check the arrows before every meal. Took me three weeks to trust them but now I’d never go back.
For anyone new: don’t overthink it. Just follow the numbers. Your body will thank you.
Cassandra Collins
December 18, 2025 AT 15:30Wait… so the government and big pharma are using CGM arrows to track us? I mean, why would they make a device that tells you when your sugar is dropping unless they wanted to control when you eat? I’ve noticed my sensor glitches right after I eat pizza. Coincidence? I think not.
Also my neighbor’s Libre showed a double-down at 2am and he ended up in the ER. That’s not science, that’s a trap.
Dave Alponvyr
December 20, 2025 AT 10:54So you’re telling me I don’t need to be a math wizard to not die? Radical.
Also, congrats on making diabetes less terrifying. I’ll take that over another pamphlet.
Tiffany Machelski
December 21, 2025 AT 22:48i just got my libre 3 and i dont know if the arrows mean the same as dexcom? i read somewhere they use different speeds? can someone help? im scared to adjust anything without being sure
James Rayner
December 22, 2025 AT 20:33It’s fascinating how a simple visual cue - arrows on a screen - can shift the entire psychology of managing a chronic condition.
Before CGMs, we were reacting to symptoms. Now we’re anticipating biology. It’s not just medicine; it’s a quiet revolution in autonomy.
And yet… we still treat it like a technical problem, not a human one. The fear of misadjusting? The guilt when you get it wrong? The loneliness of doing this alone at 3 a.m.? The tech helps - but the heart still needs a guide.
Elizabeth Bauman
December 23, 2025 AT 14:29As an American, I’m proud we’re leading the world in diabetes tech. The Endocrine Society guidelines? Pure American innovation. Other countries are still using paper logs. We’ve got AI apps, real-time arrows, and precision dosing.
Don’t let anyone tell you otherwise - this is the gold standard, and it’s made in the USA.
Arun ana
December 23, 2025 AT 17:30Just started using CGM last month. The arrows changed everything 😊
My wife says I don’t yell as much when I’m not guessing. Thank you for this guide. I printed it and put it next to my coffee maker ☕️
Josias Ariel Mahlangu
December 24, 2025 AT 19:06In my country, we do not have access to these devices. People die because they cannot afford sensors. You speak of adjusting doses like it is a privilege. It is. And it should not be.
There is no moral victory in knowing how to use arrows when others cannot even see the screen.
anthony epps
December 25, 2025 AT 16:45so if i see a double down after eating, should i still eat more carbs or just wait? i always get confused