- Toradol is a short‑acting injectable or oral NSAID used for moderate to severe pain.
- Typical adult dose is 15‑30mg every 6hours, not to exceed 5days.
- It works fast but can irritate the stomach, kidneys and bleeding risk.
- People with ulcers, kidney disease or heart problems should avoid it.
- Always follow a doctor’s prescription and watch for warning signs like unusual bruising.
What is Toradol and how does it work?
Toradol is the brand name for ketorolac tromethamine, a non‑steroidal anti‑inflammatory drug (NSAID). It belongs to the same family as ibuprofen and naproxen, but it packs a stronger punch, making it suitable for short‑term pain control after surgery, injury or dental procedures.
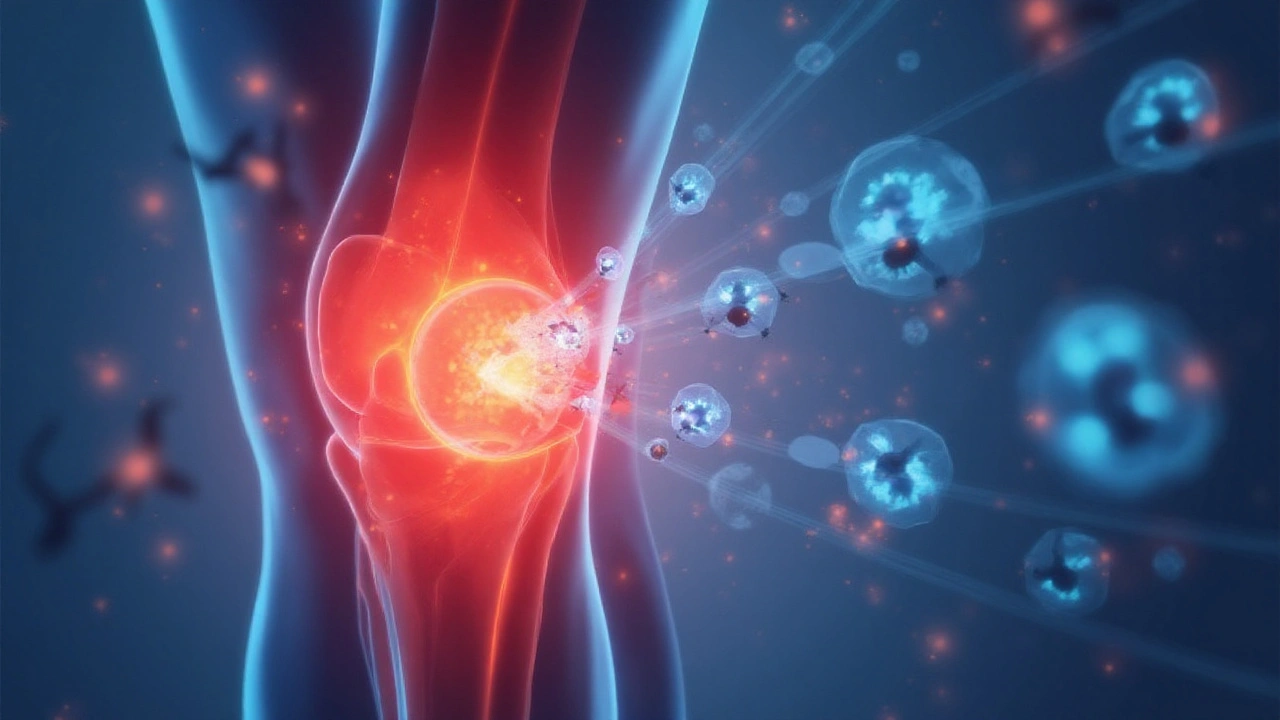
Ketorolac blocks an enzyme called cyclo‑oxygenase (COX) that produces prostaglandins - chemicals that cause inflammation, fever and pain. By cutting prostaglandin production, Toradol reduces pain quickly, often within 30 minutes when given by injection.
Because it’s powerful, regulators restrict its use to a maximum of five days. Longer exposure dramatically raises the chance of stomach ulcers, kidney injury and bleeding.
When and how is Toradol used?
Doctors prescribe Toradol for short bursts of intense pain where other NSAIDs don’t provide enough relief. Typical scenarios include:
- Post‑operative pain after orthopedic or abdominal surgery.
- Severe dental extraction pain.
- Traumatic injuries such as fractures or severe sprains.
The drug comes in three main forms:
- Intravenous (IV) or intramuscular (IM) injection - used in hospitals for rapid pain relief.
- Oral tablets (10mg, 15mg, 30mg) - for patients who can swallow and need a convenient at‑home option.
- Eye drops (ketorolac ophthalmic) - a separate formulation for post‑eye‑surgery inflammation, not covered in this guide.
For adults, the standard dosage is 15mg IV/IM every 6hours or 10mg oral every 6hours. The highest recommended daily total is 60mg (or 30mg orally). Pediatric dosing follows strict weight‑based calculations and is rarely used outside a hospital setting.
Key administration pointers:
- Never exceed five days of continuous use - the safety window is non‑negotiable.
- Take the oral tablets with food or a full glass of water to lessen stomach irritation.
- If you miss a dose, take it as soon as you remember unless it’s almost time for the next one - don’t double‑dose.
- Mixing Toradol with other NSAIDs, aspirin or blood thinners compounds bleeding risk; always disclose all meds to your clinician.

Benefits and risks you need to know
Toradol shines when you need swift, potent pain relief without resorting to opioids. Its benefits include:
- Rapid onset - pain often eases within half an hour of injection.
- Effective for both bone and soft‑tissue pain.
- Does not cause the respiratory depression or dependence associated with opioids.
But the drug carries a suite of potential downsides:
Common side effects
- Stomach upset, nausea or heartburn.
- Dizziness or headache.
- Bruising at the injection site.
Serious adverse events
- Gastrointestinal bleeding or ulceration - watch for dark stools or vomiting blood.
- Kidney injury - reduced urine output, swelling or unusual fatigue are red flags.
- Increased bleeding tendency - easy bruising, nosebleeds or prolonged bleeding from cuts.
- Heart attack or stroke risk - especially in patients with existing cardiovascular disease.
Who should avoid Toradol altogether?
- Anyone with a history of peptic ulcer disease or gastrointestinal bleeding.
- Patients with severe kidney impairment (eGFR <30mL/min/1.73m²).
- Those on anticoagulants like warfarin, direct oral anticoagulants or high‑dose aspirin.
- Pregnant women in the third trimester - it can affect fetal circulation.
If you fall into any of those categories, discuss alternative pain‑relief options with your prescriber.
Practical tips, FAQs and what to do next
Below are everyday questions people ask after hearing about Toradol, plus actionable advice.
How do I get a prescription?
Toradol is a prescription‑only medication. You’ll need to see a GP, dentist or surgeon who decides the drug is appropriate for your short‑term pain. In the UK, the prescription can be filled at any pharmacy, but the pharmacist will verify dosage and warn about interactions.
Can I take Toradol with my regular painkillers?
Mixing with other NSAIDs (ibuprofen, naproxen, aspirin) is a no‑no. If you need additional relief, a doctor may suggest acetaminophen (paracetamol) as a safer companion.
What should I do if I experience stomach pain?
Stop taking the drug immediately and contact your healthcare provider. You might need an antacid, a proton‑pump inhibitor, or a switch to a different analgesic.
Is it safe for older adults?
Older people are more prone to kidney problems and bleeding. Dosage may be reduced, and clinicians often monitor blood work closely.
How should I store Toradol?
Keep tablets in a cool, dry place out of direct sunlight. Injections should be stored at controlled room temperature (15‑30°C) and discarded after the expiry date.
What are the signs of an overdose?
Symptoms include severe stomach pain, black or tarry stools, sudden swelling, ringing in the ears (tinnitus), or confusion. If you suspect an overdose, call emergency services right away.
Can I use Toradol after a minor surgery?
Yes, but only under medical supervision. The doctor will weigh the pain‑relief benefits against the risk of bleeding, especially if you had stitches or a skin graft.
Are there any natural alternatives?
For mild‑to‑moderate pain, options like cold compresses, topical NSAID gels, or herbal anti‑inflammatories (turmeric, ginger) can help. They’re not as fast‑acting as Toradol, but they carry far fewer systemic risks.
What should I do after finishing a Toradol course?
Schedule a brief follow‑up with your prescriber to ensure there’s no lingering stomach or kidney irritation. If pain persists, ask about switching to a longer‑acting NSAID or a different class of analgesic.
Remember, the goal of Toradol is to bridge the gap between severe pain and a safer, longer‑term pain management plan. Use it exactly as directed, stay alert for warnings, and keep open communication with your healthcare team.
Next steps and troubleshooting
If you’re considering Toradol, follow this quick checklist:
- Confirm you have a valid prescription from a qualified clinician.
- Review your medical history for ulcers, kidney disease, heart conditions or anticoagulant use.
- Ask the pharmacist to explain proper storage and dosing.
- Set a reminder to stop the medication after five days.
- Track any side effects in a simple diary - note when they start, severity and any actions you took.
If you encounter unexpected symptoms, contact your GP or NHS 111 promptly. Early intervention can prevent complications and keep you on the road to recovery.


linda wood
September 21, 2025 AT 08:01My nurse had to remind me twice not to take it with ibuprofen. I thought I was being smart, combining painkillers. Turns out I was just being dumb.
LINDA PUSPITASARI
September 22, 2025 AT 17:24gerardo beaudoin
September 23, 2025 AT 09:25Joy Aniekwe
September 24, 2025 AT 23:17Latika Gupta
September 25, 2025 AT 08:50Sullivan Lauer
September 26, 2025 AT 08:23Sohini Majumder
September 27, 2025 AT 00:02tushar makwana
September 28, 2025 AT 04:41Richard Thomas
September 29, 2025 AT 07:08Matthew Higgins
September 30, 2025 AT 00:32