Ulcerative Colitis Symptom Tracker
Track Symptoms to Manage Ulcerative Colitis
Record your child's symptoms daily to identify patterns and share valuable information with their healthcare team. This tool helps you monitor disease activity and assess treatment effectiveness.
Record Today's Symptoms
Select symptoms your child is experiencing today to track disease activity.
Symptom History
Review recent symptoms to identify patterns and changes over time.
45% of days this month have reported symptoms
Based on your entries, it appears your child is experiencing moderate symptom activity. There's a pattern of symptom flares on weekdays with some relief on weekends. This pattern suggests you should consider discussing:
- Adjusting medication timing to match symptom patterns
- Stress management strategies during school days
- Additional dietary adjustments for weekdays
Your next appointment with the gastroenterologist is scheduled for next week. Be sure to share your symptom tracker results with your care team.
Important Notes
Remember, symptom trackers are a supplement to medical care, not a replacement for professional diagnosis. If your child experiences any of these red flags, seek immediate medical attention:
- Severe abdominal pain that doesn't ease with usual meds
- Persistent vomiting or inability to keep fluids down
- Rapid weight loss (>5% in a month) or signs of dehydration
- Fever above 38°C combined with bloody diarrhea
When a child is diagnosed with ulcerative colitis in children is a chronic inflammatory bowel disease that specifically affects the colon and rectum of youngsters. It brings a mix of physical discomfort and emotional stress, and families often wonder how to spot the early signs, choose the right treatment, and keep life as normal as possible.
Key Takeaways
- Watch for persistent abdominal pain, bloody stools, and growth slowdown as red flags.
- First‑line treatment usually starts with 5‑ASA drugs; steroids and biologics are added if inflammation persists.
- Nutrition, mental‑health support, and school accommodations are vital parts of a coping plan.
- Regular monitoring with blood tests, stool markers, and endoscopy helps keep the disease under control.
- Open communication between the child, parents, and healthcare team reduces anxiety and improves outcomes.
Understanding the Disease
To grasp what’s happening, it helps to see ulcerative colitis as part of the broader group called Inflammatory bowel disease (IBD). IBD also includes Crohn's disease, which can affect any part of the digestive tract. Unlike Crohn’s, ulcerative colitis is limited to the lining of the colon and always starts in the rectum, spreading upward in a continuous fashion.
Typical Symptoms in Kids
Children often present differently from adults. The most common signs include:
- Bloody or mucus‑filled stools - even a tiny amount of blood is a warning.
- Abdominal cramps that come and go, sometimes after meals.
- Urgent need to use the bathroom, leading to accidents at school.
- Unexplained weight loss or failure to gain weight.
- Fatigue that isn’t linked to lack of sleep.
- Delayed growth and puberty in chronic cases.
Because children might blame themselves or hide discomfort, parents should keep a symptom diary and note any pattern changes.
How Doctors Confirm the Diagnosis
Diagnosis hinges on three pillars: clinical history, laboratory tests, and visual inspection of the colon.
- Blood work - looks for anemia, elevated C‑reactive protein (CRP), and white‑blood‑cell count.
- Stool markers - Fecal calprotectin reliably signals intestinal inflammation.
- Endoscopy - a colonoscope lets the gastroenterologist see the inflamed mucosa and take biopsies to rule out infection.
A clear diagnosis opens the door to targeted therapy and reduces the risk of complications like toxic megacolon or colon cancer later in life.
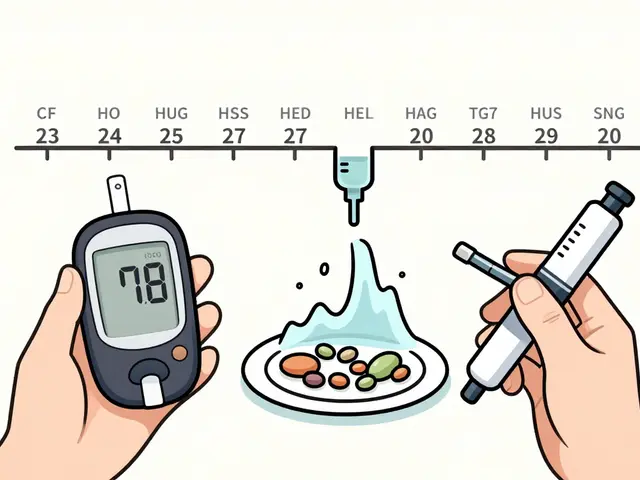
First‑Line Treatment: 5‑ASA Medications
5-ASA (mesalamine) drugs are the backbone of pediatric ulcerative colitis care. They work locally in the colon to calm inflammation without major systemic side effects.
- Oral tablets or granules - convenient for older children.
- Rectal suppositories or enemas - useful for disease limited to the rectum or left side.
Typical dosing is weight‑based; a 30‑kg child might receive 30‑45 mg/kg per day divided into two doses. Blood tests are taken every few months to watch for rare kidney issues.
When 5‑ASA Isn’t Enough: Steroids and Immunomodulators
If inflammation remains uncontrolled, doctors often turn to Corticosteroids. Prednisone or budesonide can bring rapid relief, but long‑term use is discouraged because of growth suppression, bone thinning, and mood swings.
For steroid‑dependent patients, Immunomodulators like azathioprine or methotrexate are introduced. These agents help maintain remission by dampening the immune response. Blood monitoring for liver enzymes and blood counts is essential.
Biologic Therapy - The Modern Breakthrough
Biologic therapy targets specific molecules in the inflammatory cascade. Anti‑TNF agents (infliximab, adalimumab) and anti‑integrin drugs (vedolizumab) have become standard for moderate‑to‑severe pediatric disease.
Benefits include fewer hospitalizations and the chance to grow out of steroids. Drawbacks are injection or infusion schedules and a slight increase in infection risk. Vaccinations should be up to date before starting.
Dietary Management and Lifestyle Adjustments
While no single “ulcerative colitis diet” cures the disease, certain strategies ease symptoms:
- Low‑residue meals during flare‑ups to reduce stool bulk.
- Probiotic‑rich foods (yogurt, kefir) may restore gut balance.
- Avoiding trigger foods like excessive caffeine, spicy sauces, or high‑fiber nuts when they worsen diarrhea.
- Maintaining hydration - electrolytes are lost with frequent stools.
- Regular physical activity improves mood and bowel regularity.
It’s wise to work with a pediatric dietitian who can tailor a nutrition plan that supports growth while respecting individual tolerances.
Psychological Support and Coping Strategies
The emotional toll of a chronic illness can be heavy. Kids may feel isolated at school, embarrassed by bathroom trips, or worried about their future.
- Early referral to a child psychologist familiar with chronic disease.
- Support groups - both in‑person and online - let children see peers managing similar challenges.
- School liaison - arrange for a bathroom pass, flexible deadlines, and awareness among teachers.
- Family counseling - helps parents manage stress and communicate effectively.
Simple coping tools like mindfulness breathing, journaling, and setting small daily goals can boost resilience.

Monitoring Disease Activity Over Time
Because ulcerative colitis is relapsing, regular follow‑up is non‑negotiable. The typical schedule includes:
- Clinic visit every 3‑6 months - review symptoms, growth chart, and medication side‑effects.
- Blood work (CBC, CRP, liver enzymes) at each visit.
- Fecal calprotectin every 6 months or when symptoms change.
- Surveillance colonoscopy every 1‑2 years after 8 years of disease duration to screen for dysplasia.
Staying ahead of flares reduces emergency department visits and prevents complications.
Comparison of Common Treatment Options
| Medication | Mechanism | Typical Use | Common Side Effects | Age Approved |
|---|---|---|---|---|
| 5‑ASA (mesalamine) | Topical anti‑inflammatory | First‑line mild‑moderate disease | Headache, nausea, rare kidney issues | 6 years+ |
| Corticosteroids (prednisone) | Systemic immunosuppression | Induction of remission during flare | Weight gain, mood swings, bone loss | 2 years+ |
| Immunomodulators (azathioprine) | Inhibits DNA synthesis in immune cells | Maintenance for steroid‑dependent cases | Liver toxicity, low blood counts | 5 years+ |
| Biologics (infliximab) | Anti‑TNF monoclonal antibody | Moderate‑severe disease, refractory cases | Infusion reactions, infections | 6 years+ |
| Dietary therapy | Modifies gut microbiome & stool bulk | Adjunct to meds, symptom control | Potential nutrient deficiencies if not supervised | All ages (with dietitian guidance) |
Practical Tips for Daily Life
Putting knowledge into routine makes a big difference. Here are actionable ideas:
- Medication tracker - use a phone app or pillbox to avoid missed doses.
- Keep a symptom log - note stool frequency, blood presence, and pain level. Share it with the doctor before appointments.
- Pack a ‘go‑bag’ for school: spare underwear, a small bottle of water, and a note for teachers explaining the condition.
- Schedule regular growth checks - height and weight trends are early signs of nutritional gaps.
- Plan family meals with low‑residue options during flares, and re‑introduce fiber gradually when remission returns.
When to Seek Immediate Help
Even with good control, certain red‑flag signs demand urgent medical attention:
- Severe abdominal pain that doesn’t ease with usual meds.
- Persistent vomiting or inability to keep fluids down.
- Rapid weight loss (>5 % in a month) or signs of dehydration.
- Fever above 38 °C combined with bloody diarrhea.
- Sudden change in bowel habits lasting more than 48 hours.
Calling the gastroenterology clinic or going to the emergency department can prevent complications like toxic megacolon.
Looking Ahead: Research and Future Directions
Scientists are exploring novel approaches that may reshape pediatric care in the next decade:
- Microbiome‑targeted therapies - fecal microbiota transplant (FMT) trials show promise for refractory cases.
- Selective Janus kinase (JAK) inhibitors - oral pills that block specific inflammation pathways.
- Personalized medicine - using genetic markers to predict which drug a child will respond to best.
Staying informed about clinical trials can give families early access to cutting‑edge treatments.
What are the first signs of ulcerative colitis in a child?
Typical early signs include bloody or mucus‑filled stools, abdominal cramps, urgency to use the bathroom, unexplained weight loss, and fatigue. Parents should note any pattern changes and discuss them with a pediatrician.
Is ulcerative colitis curable in children?
Currently there is no cure, but many children achieve long‑term remission with medication, diet, and proper monitoring. Early, aggressive treatment can keep the disease under control and allow normal growth.
How often should my child have colonoscopies?
Guidelines suggest a surveillance colonoscopy every 1‑2 years after 8 years of disease duration, especially if the child has extensive colitis. Your gastroenterologist will personalize the schedule based on inflammation severity.
Can my child still play sports?
Yes. Most children can continue sports as long as they manage hydration, monitor fatigue, and have quick bathroom access if needed. Discuss any restrictions with the care team during flare‑ups.
What dietary changes help during a flare?
A low‑residue (low‑fiber) diet reduces stool bulk. Avoid nuts, seeds, raw vegetables, and high‑fat foods. Incorporate easily digestible proteins, cooked carrots, peeled apples, and plenty of clear fluids. Work with a dietitian for a balanced plan.


Steven Young
October 22, 2025 AT 12:49Kids with ulcerative colitis are often misdiagnosed because doctors ignore subtle red flags and focus on the usual suspects. The lack of transparency in pharmaceutical trials is alarming and fuels my distrust of the mainstream medical narrative. Parents should demand independent testing before committing to any drug regimen.
Kelly Brammer
October 30, 2025 AT 19:49It is morally reprehensible to let a child suffer in silence while ignoring these clear warning signs. Ethical responsibility demands that caregivers prioritize early detection and honest communication with healthcare providers.
Oliver Johnson
November 8, 2025 AT 03:49America should stand strong and protect its children from these invasive foreign drug trials. The so‑called "standard of care" often hides profit motives behind a mask of science. I challenge anyone to prove that these medications are truly safe for our youth.
Sireesh Kumar
November 16, 2025 AT 11:49Listen up, folks – I’ve read every guideline and then some, so let me break it down for you. First‑line 5‑ASA is fine, but only if you keep a strict medication diary and never skip a dose. If the disease flares, jump straight to steroids under strict supervision, and don’t forget the follow‑up labs.
Ritik Chaurasia
November 24, 2025 AT 19:49From an Indian perspective, dietary balance is crucial; spices like turmeric can be anti‑inflammatory but must be used wisely. Parents should coordinate with a dietitian to integrate culturally appropriate meals that support growth. Aggressive monitoring of blood work will keep complications at bay.
Taylor Haven
December 3, 2025 AT 03:49When we examine the first signs of ulcerative colitis in a child, we must consider the broader sociopolitical context that shapes medical practice. The blood in stool is not merely a symptom; it is a signal that the system has failed to provide timely diagnostics. Persistent abdominal pain should trigger an immediate referral, yet many practitioners dismiss it as ordinary indigestion due to entrenched biases. Moreover, the escalation to biologics is often delayed because insurance companies lobby to keep costs low, compromising the child's right to optimal care. Parents are left navigating a labyrinth of appointments, each demanding its own set of paperwork, which is a direct consequence of bureaucratic overreach. The recommended growth monitoring, while essential, is seldom enforced uniformly across regions, leading to disparities that echo larger social inequities. Nutritional interventions, though highlighted, are frequently overlooked in favor of pharmaceutical solutions, a trend that reflects the profit-driven nature of modern healthcare. The emphasis on mental‑health support is commendable, yet schools are reluctant to allocate resources, forcing families to seek private services. This further widens the gap between affluent and under‑privileged families. A child’s desire to participate in sports should never be curtailed by fear of flare‑ups; instead, coaches must be educated on proper hydration and restroom access. The surveillance colonoscopy schedule, mandated after eight years of disease, is another checkpoint that reveals how the system prioritizes long‑term data collection over immediate quality of life. In addition, the emergence of fecal calprotectin testing offers a non‑invasive monitoring tool, but its availability is uneven, reflecting a fragmented approach to care. Children’s resilience is remarkable, but it should not be taken as a justification for lax treatment protocols. We must advocate for consistent guidelines, transparent drug pricing, and equitable access to multidisciplinary teams. Ultimately, the fight against ulcerative colitis in children is not just medical; it is a battle for justice, equity, and the preservation of childhood itself.
Mary Keenan
December 11, 2025 AT 11:49Sounds like a lot of red tape.
Ben Collins
December 19, 2025 AT 19:49Wow, another endless list of tips – because we all have the time to become nutritionists, psychologists, and gastro‑pros overnight. But hey, if you love juggling meds, diet plans, and school talks, you’re basically a superhero. Grab a cape next time you refill the prescription.
Denver Bright
December 28, 2025 AT 03:49I guess I’ll just sit back and let everyone else deal with the chaos…
Kelli Benedik
January 5, 2026 AT 11:49✨OMG, this article is a rollercoaster of feels!💥 The part about low‑residue meals during flares made me think of my grandma’s bland soup, and I’m crying 😂. But seriously, the biopsies sound scarier than my last horror movie night 🌙. Let’s all hug our kids tighter and remember the power of probiotics 🍦.
cariletta jones
January 13, 2026 AT 19:49Great vibe! Keep sharing the optimism – it really helps families stay hopeful.
Kevin Hylant
January 22, 2026 AT 03:49Monitoring stool frequency and blood presence daily gives a clear picture of disease activity. Regular blood tests catch anemia early and prevent complications. Staying on schedule with medication reduces the risk of flare‑ups and supports growth.
Holly Green
January 30, 2026 AT 11:49Everyone should know that early aggressive treatment can lead to remission, not just symptom management. It's important to follow the colonoscopy schedule to catch any early signs of dysplasia. Staying informed about clinical trials gives families access to cutting‑edge therapies.
Craig E
February 7, 2026 AT 19:49Reflecting on the journey of a child with ulcerative colitis, one sees a tapestry woven from medical science, familial love, and societal support. The delicate balance between treatment efficacy and quality of life mirrors the philosophical quest for harmony. Let us contemplate how each stakeholder can contribute to a more compassionate care model.
Marrisa Moccasin
February 16, 2026 AT 03:49Did you know-some hidden labs are deliberately withholding data?!! This is why we must stay vigilant; the truth is out there, and it’s being suppressed!!!