When you’re managing diabetes, especially type 1, getting your blood sugar right isn’t just about taking insulin-it’s about matching it to your life. Basal-bolus insulin therapy is the closest thing we have to a natural pancreas. It’s not magic, but when done right, it gives you freedom: eat when you want, move when you feel like it, and still stay in range. But it’s also complex. Too little insulin, and your numbers creep up. Too much, and you’re fighting low blood sugar. So how do you actually get it right?
What Basal-Bolus Insulin Really Means
Basal-bolus isn’t just two types of insulin-it’s two roles. Basal insulin is your background dose. It works all day, every day, keeping your blood sugar steady between meals and overnight. Think of it like a slow drip of insulin that keeps your liver from dumping too much glucose into your bloodstream. Bolus insulin is your mealtime dose. It’s fast-acting. You take it right before or after eating to cover the carbs you’re consuming and to fix high blood sugar. This system was proven in the 1993 Diabetes Control and Complications Trial (DCCT). People who used intensive insulin therapy-basal-bolus-cut their risk of eye, kidney, and nerve damage by up to 76%. That’s not a small win. Since then, it’s been the gold standard for type 1 diabetes. But it’s also recommended for type 2 diabetes when pills and basal insulin alone aren’t enough.How to Calculate Your Total Daily Insulin Need
Start with your weight. That’s your foundation. The standard formula? 0.5 units of insulin per kilogram of body weight. So if you weigh 70 kg (about 154 pounds), your total daily insulin need is roughly 35 units. Some people use a simpler version: divide your weight in pounds by 4. A 160-pound person? That’s 40 units total per day. But this is just a starting point. Your actual need might be higher if you’re insulin resistant, or lower if you’re very active or lean. The range? Between 0.4 and 1.0 units per kg. That’s a wide band, and it’s intentional. You’ll fine-tune this over weeks, not days.Splitting the Dose: Basal vs. Bolus
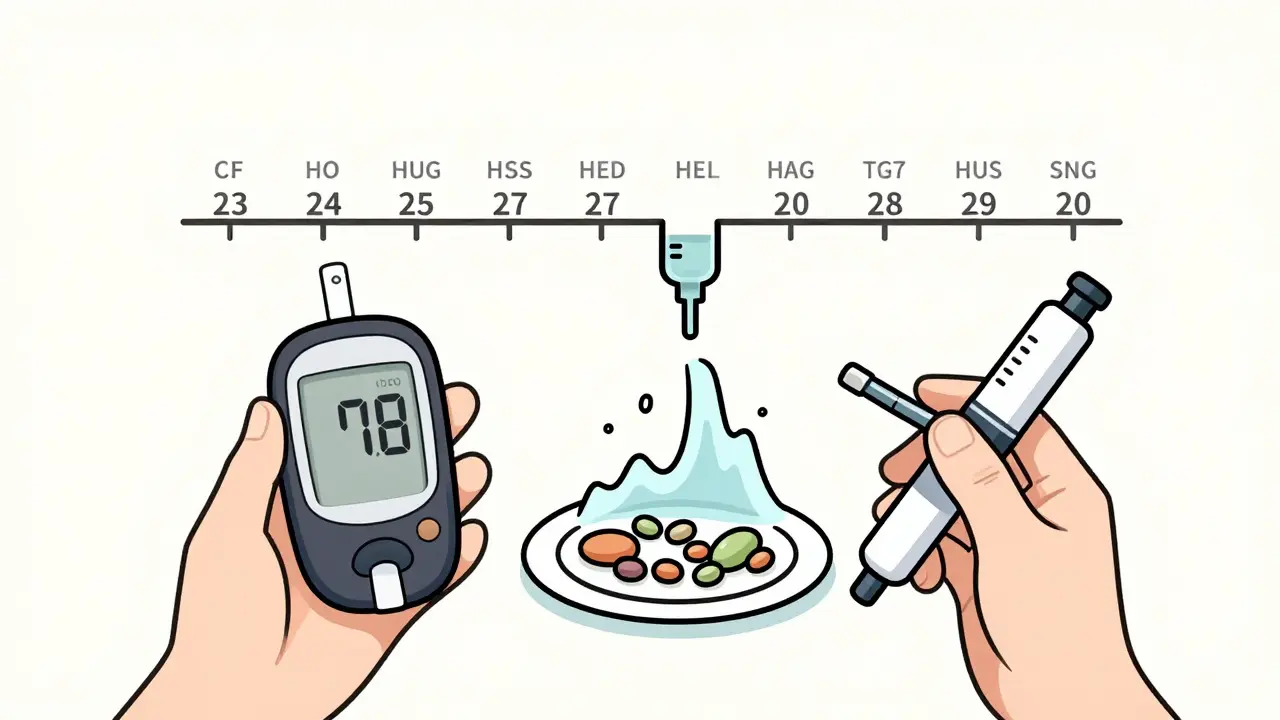
Now, divide that total. For most people with type 1 diabetes, half goes to basal, half to bolus. That’s 50/50. So if your total is 40 units, 20 go to basal, 20 to bolus. Basal insulin is usually taken once or twice a day-long-acting types like glargine, detemir, or degludec. Bolus insulin is rapid-acting: lispro, aspart, or glulisine. You take it with every meal or snack that has carbs. The 50/50 split isn’t arbitrary. It’s based on how much insulin healthy pancreases naturally release throughout the day. Your body makes about half its insulin as background, half as mealtime bursts. Basal-bolus tries to copy that.Figuring Out Your Bolus Dose
Your bolus dose isn’t just one number. It’s two parts: carb coverage and correction. For carb coverage, use the 500 Rule. Take your total daily insulin (TDIR), divide it by 500. That gives you how many grams of carbs one unit of insulin covers. If your TDIR is 50 units, 500 ÷ 50 = 10. So one unit covers 10 grams of carbs. Eat 45 grams of carbs? That’s 4.5 units of insulin. For correction, use the 1700 Rule. Take your TDIR and divide by 1700. That tells you how much one unit of insulin lowers your blood sugar. If your TDIR is 40 units, 1700 ÷ 40 = 42.5. So one unit drops your blood sugar by about 43 mg/dL. If your glucose is 200 mg/dL and your target is 120, you’re 80 points high. 80 ÷ 42.5 ≈ 1.9 units. Round to 2 units. Add the two together: carb dose + correction dose = your total bolus. That’s your mealtime number.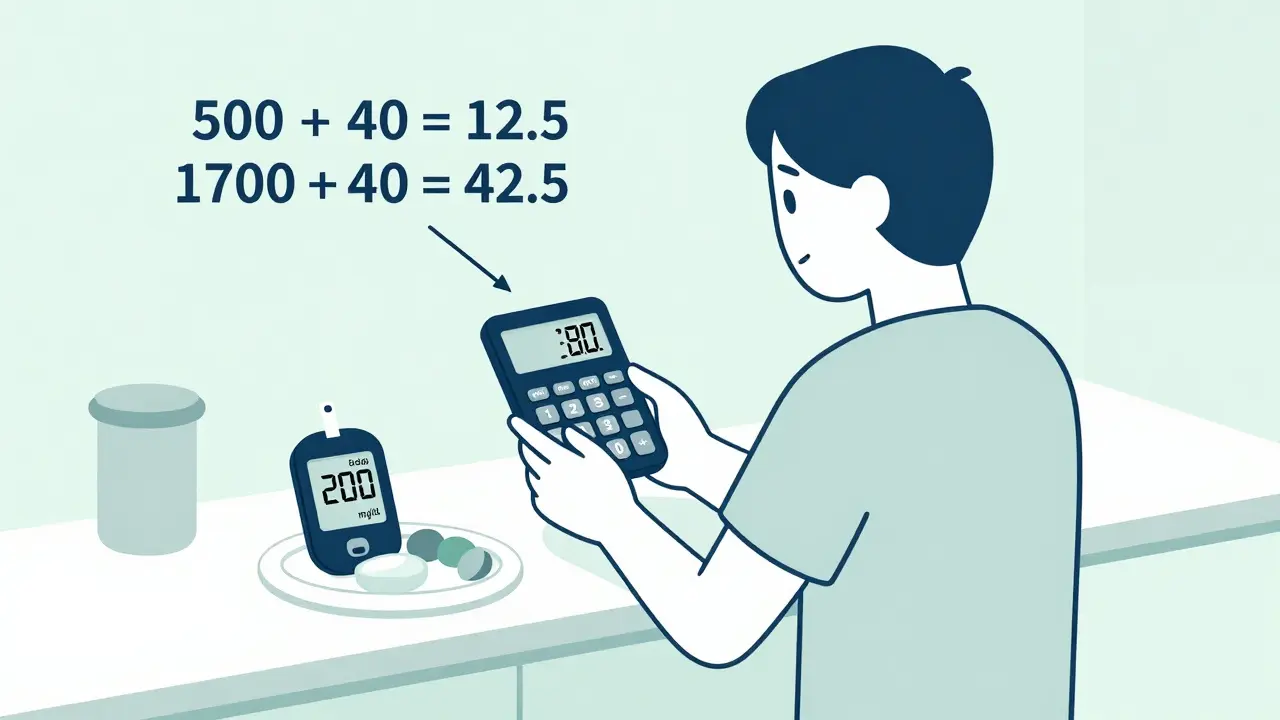
Starting Basal Insulin: The Safe Way
Don’t guess your basal dose. Start low. The American Diabetes Association recommends 10 units a day or 0.1-0.2 units per kg. So if you weigh 70 kg, start with 7-14 units. Take it at the same time every day-usually bedtime or morning. Check your fasting blood sugar every morning. Your goal? 80-130 mg/dL. If your fasting number is above 130, increase basal by 2 units every 2-4 days. Don’t rush. Too fast, and you risk lows later. If it’s below 80, drop by 1-2 units. It’s slow work. But once you hit your target, your baseline is stable. That’s when bolus dosing gets easier.Why People Struggle-and How to Fix It
The biggest hurdle isn’t math. It’s consistency. Most people get stuck on carb counting. Estimating 45 grams of pasta? You might be off by 15. That’s a 3-unit error. That’s a spike. Or you forget to correct for a high reading before dinner. Suddenly, your post-meal number is 250. A 2022 survey found 68% of patients find dose calculations hard. But here’s the fix: use a log. Write down what you ate, your pre-meal glucose, your bolus dose, and your result two hours later. Look for patterns. If your lunch numbers are always high, maybe your carb ratio is too high. If your bedtime is low, maybe your basal is too much. Certified Diabetes Care and Education Specialists (CDCES) are your best ally. Studies show patients who work with them have 37% better outcomes. Don’t try to do this alone. Ask your clinic for a referral.Basal-Bolus vs. Other Options
Some people use premixed insulin-like 70/30 or 50/50 blends. It’s simpler: two shots a day. But it’s rigid. You eat at the same time, same carbs, every day. No flexibility. The ORBIT study showed basal-bolus lowered HbA1c by 0.4% more than premixed-but caused 1.3 times more low blood sugar events. Basal-only insulin? Great for type 2 patients who just need to lower fasting sugars. But if your after-meal numbers are sky-high, basal-only won’t fix it. Basal-bolus adds the missing piece. The trade-off? Basal-bolus needs 4-5 injections a day. Premixed? 2. Basal-only? 1. But basal-bolus gives you control. You can skip a meal without crashing. You can have dessert. You can exercise and adjust. That’s worth the effort for most people with type 1.What’s New in Basal-Bolus Therapy
Technology is changing this game. Hybrid closed-loop systems-like Tandem’s Control-IQ or Medtronic’s MiniMed 780G-now use continuous glucose monitors (CGM) to auto-adjust basal insulin. Some even suggest bolus doses. In 2023, users saw an extra 2.1 hours per day in target range compared to manual dosing. New insulins are coming too. Novo Nordisk’s insulin icodec, expected in 2025, lasts up to 40 hours. That means one weekly shot for basal. Less frequent dosing. Less stress. But here’s the catch: these tools don’t replace learning. You still need to know how to count carbs. You still need to understand insulin action. The machine helps, but you’re still the pilot.
Who It Works For-and Who It Doesn’t
Basal-bolus shines for people who:- Have type 1 diabetes
- Want flexibility in meals and schedule
- Struggle with high post-meal sugars
- Are motivated to learn and track
- Have cognitive or dexterity issues
- Can’t reliably check blood sugar
- Are overwhelmed by numbers
- Have limited access to education or support
Real Stories, Real Results
One user on the ADA forum switched from twice-daily premixed insulin to basal-bolus. In six months, their A1c dropped from 8.5% to 6.7%. They said it took three months to get comfortable with carb counting-but the freedom was worth it. Another, on Reddit, said: “I’ve been on basal-bolus for two years and still second-guess my doses.” That’s normal. Even experts adjust. It’s not about perfection. It’s about progress. The T1D Exchange Registry found 78% of users felt their control improved. But 45% said the burden was high. The key? Support. Education. Patience.Your Next Steps
If you’re starting basal-bolus:- Get your weight in kilograms.
- Calculate TDIR: weight × 0.5.
- Split it 50/50: basal = half, bolus = half.
- Start basal at 10 units or 0.1-0.2 units/kg.
- Use 500 ÷ TDIR for carb ratio.
- Use 1700 ÷ TDIR for correction factor.
- Log every meal, dose, and result.
- See a CDCES for structured training.
When to Call Your Doctor
If you’re having frequent lows (below 70 mg/dL) without clear cause, or if your fasting sugars stay above 160 mg/dL after two weeks of basal adjustments, it’s time to talk. You might need a different insulin type, a change in timing, or help with your carb counting. And if you’re feeling overwhelmed? You’re not alone. Basal-bolus is powerful, but it’s not meant to be a solo mission. Ask for help. Use the tools. Keep going.What’s the difference between basal and bolus insulin?
Basal insulin is long-acting and works all day to keep your blood sugar steady between meals and overnight. Bolus insulin is fast-acting and taken at meals to cover carbs and correct high blood sugar. Together, they mimic how a healthy pancreas works.
How do I calculate my insulin dose for meals?
Use two numbers: your carb ratio and your correction factor. Your carb ratio is 500 divided by your total daily insulin dose. That tells you how many grams of carbs one unit covers. Your correction factor is 1700 divided by your total daily insulin dose-that’s how many points one unit lowers your blood sugar. Add the carb dose and correction dose together for your total bolus.
Can I use basal-bolus insulin if I have type 2 diabetes?
Yes. If you’re on oral meds or basal insulin alone and still not hitting your A1c target, your doctor may recommend adding bolus insulin. Basal-bolus is especially helpful if your blood sugar spikes badly after meals.
How long does it take to get good at basal-bolus dosing?
Most people get comfortable within 4 to 12 weeks. It takes time to learn carb counting, recognize patterns, and adjust doses safely. Don’t rush. Use a log, ask for help, and celebrate small wins.
Is basal-bolus insulin more expensive?
Yes. You’re using two types of insulin instead of one, and you may need more frequent supplies like test strips or CGM sensors. In the U.S., out-of-pocket insulin costs average $550 per month. But better control can reduce long-term costs from complications like kidney disease or nerve damage.
What if I miss a bolus dose?
If you realize you missed it within 2 hours of eating, you can still take a reduced dose. Use your correction factor to bring your sugar down. If it’s been longer, don’t double up. Instead, monitor your sugar closely and adjust your next dose. Always talk to your care team about missed doses.
Can I switch from premixed to basal-bolus insulin?
Yes, but do it under medical supervision. Your doctor will calculate your new basal and bolus doses based on your current total insulin use. You’ll likely need more frequent monitoring at first. Many people find the switch improves control, even if it feels more complicated at first.


Martin Spedding
December 17, 2025 AT 15:04Raven C
December 18, 2025 AT 13:07amanda s
December 20, 2025 AT 08:11Salome Perez
December 21, 2025 AT 10:16Kent Peterson
December 22, 2025 AT 11:07Jane Wei
December 22, 2025 AT 18:59Nishant Desae
December 24, 2025 AT 03:21Jonathan Morris
December 24, 2025 AT 11:55Jessica Salgado
December 25, 2025 AT 09:26Chris Van Horn
December 27, 2025 AT 07:49Virginia Seitz
December 27, 2025 AT 12:59Peter Ronai
December 28, 2025 AT 21:16Michael Whitaker
December 30, 2025 AT 11:52Patrick A. Ck. Trip
December 31, 2025 AT 21:19