Serotonin Syndrome Risk Checker
Medication Combination Risk Assessment
This tool estimates your risk of serotonin syndrome based on your current medications and health factors. Always consult your doctor before making any medication changes.
Your Risk Assessment
Recommended Actions:
Note: This assessment is for informational purposes only. Always consult your healthcare provider.
Combining SSRIs and opioids might seem harmless if you’re just following your doctor’s prescriptions. But for thousands of people, this common mix can trigger a dangerous, sometimes deadly reaction called serotonin syndrome. It doesn’t happen because someone took too much - it happens because two perfectly legal medications, when used together, overload your brain’s serotonin system. And most people don’t know it’s even possible.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t an allergy or a side effect you can predict by how you feel after one pill. It’s a toxic buildup of serotonin - a chemical your brain uses to control mood, movement, and body temperature. When too much serotonin floods your system, your nerves go into overdrive. Symptoms can start within hours, and they range from annoying to life-threatening.You might feel shivering you can’t stop, your muscles twitch uncontrollably, or your heart races without reason. In worse cases, your body temperature spikes above 40°C (104°F), your muscles lock up like a statue, and you become confused or unresponsive. Left untreated, severe serotonin syndrome can lead to seizures, kidney failure, or death. About 1 in 10 people with the most serious form don’t survive.
The good news? It’s preventable. The bad news? Many doctors still miss it. Emergency rooms misdiagnose serotonin syndrome as something else - like a drug overdose, heatstroke, or even a psychiatric crisis - nearly half the time. That delay can cost lives.
Which Opioids Are Dangerous With SSRIs?
Not all opioids are created equal when it comes to serotonin risk. Some are fine. Others are ticking time bombs.High-risk opioids: Tramadol, methadone, and pethidine (meperidine). These don’t just relieve pain - they directly block serotonin from being cleared out of your brain. Tramadol, for example, is 30 times stronger than morphine at interfering with serotonin. That’s why, out of every 100 reported serotonin syndrome cases involving opioids, nearly 40 involve tramadol. The FDA has flagged this combination as a major concern.
Lower-risk opioids: Morphine, oxycodone, hydromorphone, and buprenorphine. These work mainly on pain receptors without significantly affecting serotonin. If you’re on an SSRI and need strong pain relief, these are the safer choices - if your doctor knows to pick them.
Even codeine, long thought to be safe, has been linked to serotonin syndrome in people already taking SSRIs like paroxetine. And fentanyl? It doesn’t block serotonin in lab tests, but real-world reports show over 120 cases of serotonin syndrome linked to it. Science doesn’t always match reality.
Which Antidepressants Carry the Highest Risk?
SSRIs aren’t all the same either. Fluoxetine (Prozac) sticks around in your body for weeks - even after you stop taking it. Its active metabolite, norfluoxetine, can linger for up to 16 days. That means if you switch from fluoxetine to another medication, you’re still at risk for days or even weeks. Sertraline, on the other hand, clears out in about a day. That’s a big difference when planning a medication change.SNRIs like venlafaxine (Effexor) are even more likely to cause problems than SSRIs because they boost both serotonin and norepinephrine. And MAOIs? Those are the most dangerous of all. Mixing an MAOI with any opioid can be fatal, even at normal doses. That’s why doctors require a full 14-day gap - or five weeks if you were on fluoxetine - before switching to any other antidepressant or painkiller.

Who’s Most at Risk?
It’s not just about the drugs you take - it’s about your body’s ability to handle them.Older adults are at higher risk. People over 65 take, on average, 31% more medications than younger people. More pills = more chances for bad interactions. That’s why the American Geriatrics Society specifically warns against prescribing tramadol to seniors already on SSRIs.
People with liver or kidney problems are also vulnerable. If your body can’t break down drugs properly, even a normal dose can become toxic. The same goes for people with a genetic variation called CYP2D6 poor metabolism. These individuals process tramadol and other opioids much slower, leading to dangerous buildup. Studies show they’re over three times more likely to develop serotonin syndrome.
And then there’s the hidden risk: recent dose changes. Most cases happen within hours of starting a new opioid or increasing the dose of an existing one. That’s why doctors need to watch you closely during those first few days.
How to Prevent It - Practical Steps
Prevention isn’t about avoiding all opioids or SSRIs. It’s about making smart choices.- Ask your doctor: “Is this opioid safe with my antidepressant?” Don’t assume it is. Bring a list of every medication you take - including over-the-counter ones like dextromethorphan (found in cough syrup), which also raises serotonin.
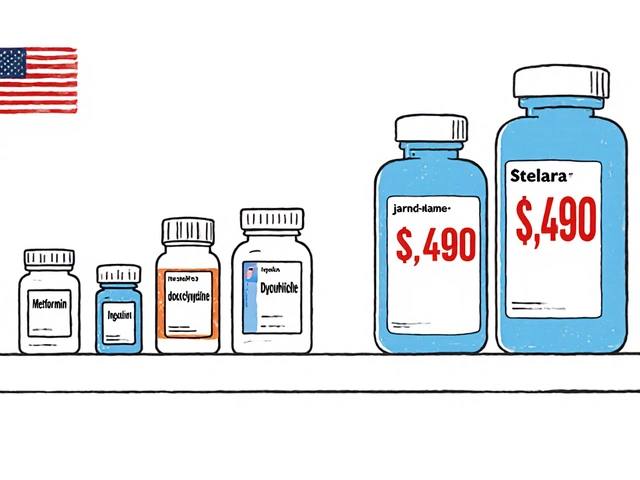
- Push for safer alternatives. If you’re on an SSRI and need pain relief, ask for morphine, oxycodone, or hydromorphone instead of tramadol or methadone. Many doctors default to tramadol because it’s cheaper and thought to be “milder.” It’s not.
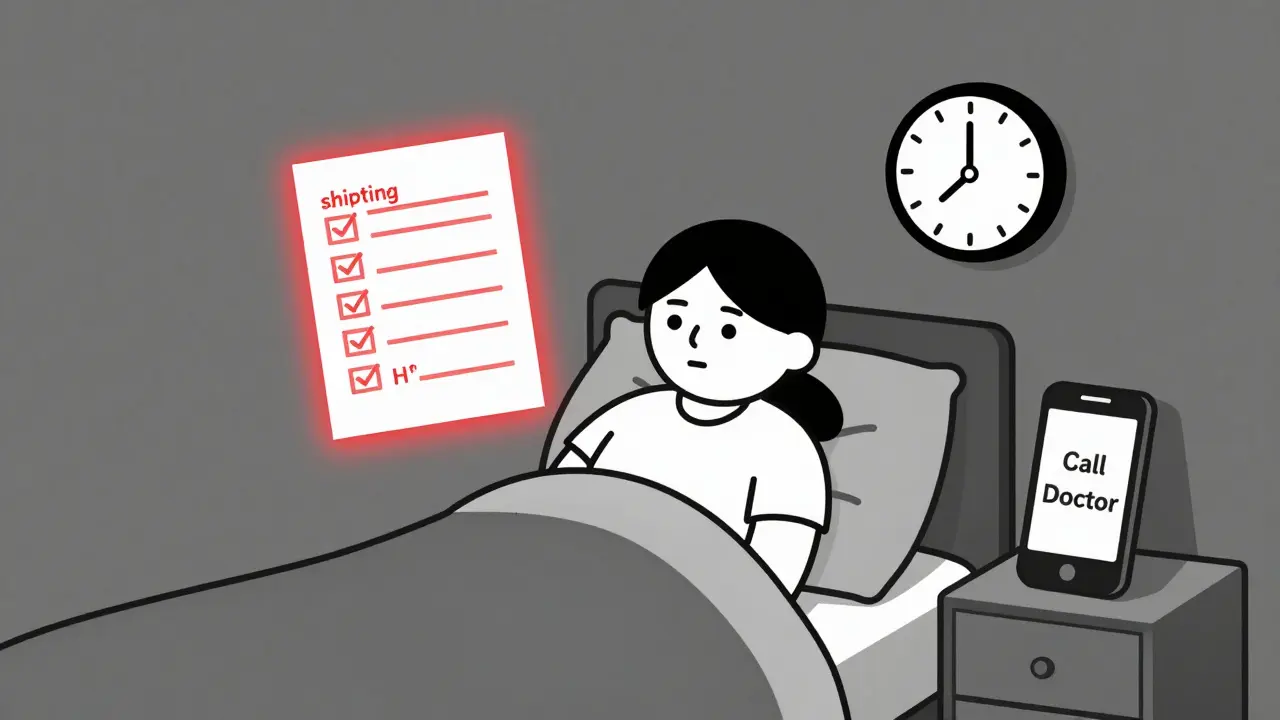
- Watch for early signs. Keep a simple checklist: shivering, muscle twitches, rapid heartbeat, sweating, confusion, or diarrhea. If you notice two or more of these after starting a new painkiller, stop it and call your doctor immediately.
- Don’t stop or start meds on your own. Even switching from one SSRI to another can trigger serotonin syndrome if there’s no clean break. Always follow your doctor’s washout schedule.
- Check your pharmacy’s alerts. Many pharmacies now flag high-risk combinations. If your pharmacist calls you about a new prescription, listen. They’ve seen this before.
What Happens If It Goes Wrong?
If serotonin syndrome is suspected, the first step is simple: stop all serotonergic drugs immediately. That includes your SSRI, your opioid, and any cough medicine with dextromethorphan.For mild cases, symptoms often fade within 24 to 72 hours once the drugs are out of your system. But severe cases need emergency treatment. Doctors use benzodiazepines like diazepam to calm muscle rigidity and agitation. For fever above 41°C, they cool you down with ice packs and IV fluids. And they give cyproheptadine - a drug that blocks serotonin receptors - to reverse the effects. The standard dose? 12 mg right away, then 2 mg every two hours if needed.
Hospitalization is often required. In one case from a UK hospital, a 68-year-old woman on sertraline developed a fever of 40.2°C and spontaneous muscle clonus just 12 hours after starting tramadol. She needed intensive care. She survived - but only because the ER team recognized it fast.
What’s Changing in 2026?
The medical world is waking up. The FDA now requires opioid medication guides to include serotonin syndrome warnings. The European Medicines Agency forced tramadol labels to carry stronger alerts. And hospitals are upgrading their systems: Kaiser Permanente cut dangerous tramadol-SSRI prescriptions by 87% after adding automatic alerts in their electronic records.Next up? Real-time risk scoring. Epic Systems, the biggest electronic health record provider, is rolling out new tools in 2024 that analyze your genetics, liver function, and current meds to predict serotonin risk before a prescription is even written. In the UK, the National Poisons Information Service is training more pharmacists to spot early signs - because they’re often the first to notice.
Research is also moving toward blood tests that could detect serotonin syndrome before symptoms get bad. A £2.4 million NIH-funded study is underway to find biomarkers that signal trouble before the body shuts down.
Final Word: Know the Signs, Speak Up
You’re not overreacting if you’re worried about your meds. Serotonin syndrome isn’t rare - it’s just underdiagnosed. Every month, hospital pharmacists in the UK and US report seeing two to three cases from tramadol and SSRIs alone. Many of these patients thought they were doing everything right.If you’re on an SSRI and your doctor prescribes an opioid, ask: “Is this the safest option?” If they say yes without checking your full med list, ask again. If you feel strange after starting a new painkiller - shivering, twitching, sweating, or your heart racing - don’t wait. Call your doctor or go to urgent care. Serotonin syndrome doesn’t wait.
Can I take tramadol with an SSRI if I’m careful?
No. Even at low doses, tramadol combined with SSRIs carries a high risk of serotonin syndrome. Studies show it’s over four times more likely to cause the condition than morphine. There are safer painkillers available. Don’t risk it.
How long after stopping an SSRI is it safe to start an opioid?
It depends on the SSRI. For sertraline or escitalopram, wait at least 5 days. For fluoxetine, wait 5 weeks because it stays in your system much longer. Never start an opioid without checking with your doctor - and never assume the SSRI is fully out of your system just because you stopped taking it.
Is serotonin syndrome the same as an opioid overdose?
No. An opioid overdose causes slow breathing, drowsiness, and unconsciousness. Serotonin syndrome causes muscle rigidity, shivering, rapid heart rate, and high body temperature. They’re opposite in many ways. Mistaking one for the other delays life-saving treatment.
Can I take over-the-counter cough medicine with my SSRI?
Avoid cough syrups with dextromethorphan. It’s a serotonergic drug and can trigger serotonin syndrome when combined with SSRIs. Look for alternatives like guaifenesin-only formulas or non-sedating options. Always check the active ingredients.
What should I do if I think I’m having serotonin syndrome?
Stop taking all serotonergic medications immediately. Call your doctor or go to the nearest emergency room. Tell them you’re on an SSRI and an opioid, and you’re experiencing symptoms like muscle twitching, shivering, or a rapid heartbeat. Don’t wait for symptoms to worsen.



Mindee Coulter
January 27, 2026 AT 14:06Just had my doc switch me from tramadol to oxycodone last month after I mentioned I was on sertraline. He didn’t even blink. Took me 3 years to get him to listen. Seriously, if your doctor doesn’t know this, find a new one.
Colin Pierce
January 28, 2026 AT 00:32As a pharmacist, I see this every week. People come in with tramadol and fluoxetine and think they’re fine because ‘it’s just a pain pill.’ Then they get shaky and confused and blame the weather. We flag it, we call, we scream. But patients rarely listen until it’s too late. Please, if you’re on an SSRI, ask about serotonin risk before filling any new script.
Anna Lou Chen
January 28, 2026 AT 17:40Let’s not romanticize the pharmacological monoculture. The entire biomedical paradigm is built on reductionist pharmacokinetic models that ignore emergent neurochemical synergies. SSRIs and opioids aren’t just ‘drugs’-they’re perturbations in a homeostatic network governed by serotonergic-μ-opioid crosstalk. Tramadol’s dual reuptake inhibition + weak agonism creates a non-linear feedback loop that defies clinical heuristics. We’re treating symptoms while the system collapses. This isn’t about ‘safe alternatives’-it’s about dismantling the pharmacological colonialism that prioritizes cost over complexity.
And don’t get me started on how the FDA’s ‘warnings’ are performative gestures to appease liability lawyers while the real problem-systemic prescriber ignorance-remains unaddressed. The system doesn’t want you to know. It wants you to comply.
Real prevention? Genetic screening before prescribing. Real prevention? Ban tramadol from formularies entirely. Real prevention? Stop treating patients like data points and start treating them like organisms with metabolisms, not just pill containers.
And yes, I’ve seen three cases. Two died. One is now permanently neurologically impaired. This isn’t theoretical. It’s a slow-motion massacre disguised as medical care.
Brittany Fiddes
January 29, 2026 AT 16:04Oh, so now it’s ‘safer opioids’? LOL. You think morphine is safe? Have you seen the opioid epidemic? The whole system is rigged. Pharma pushed tramadol because it was cheap and profitable. Now they’re pushing ‘safer’ opioids because they need a new profit stream. It’s all the same game. They don’t care if you live or die-they care if you keep buying.
And why is no one talking about how the FDA is in bed with Big Pharma? The ‘warnings’ are toothless. They don’t ban anything. They just slap a label on it and call it a day. Meanwhile, your doctor’s still getting kickbacks from reps in white coats. Wake up.
I know someone who died from this. They were on sertraline and ‘just’ took oxycodone for a back injury. The ER said it was ‘sepsis.’ It wasn’t. It was serotonin syndrome. They didn’t even test for it.
They’re lying to you. All of them.
John Rose
January 30, 2026 AT 08:46This is one of the most important posts I’ve read in years. I’ve been on fluoxetine for 8 years and was just prescribed oxycodone for a herniated disc. I didn’t know any of this. I printed this out and took it to my doctor. He actually listened. We switched to hydromorphone. I’m alive because of this.
If you’re reading this and you’re on an SSRI-don’t wait. Ask. Even if it feels awkward. Your life matters more than your doctor’s convenience.
Rhiannon Bosse
January 31, 2026 AT 05:49So let me get this straight… the same people who told us Vicodin was safe are now telling us morphine is ‘safer’? 😂 Meanwhile, your pharmacy’s AI system is probably flagging your meds but your doctor’s still on a 1998 Windows XP computer yelling ‘I’ve been doing this for 30 years!’ 💀
And don’t even get me started on dextromethorphan. You think your cough syrup is innocent? Nah. That stuff’s basically liquid ecstasy with a side of serotonin overload. 🤯
Also, I saw a TikTok where a guy said he felt ‘weird’ after mixing Lexapro and tramadol… then he went to the ER and they told him he was ‘just anxious.’ He died 4 hours later. 😔
Y’all need to stop trusting doctors like they’re gods. They’re just humans with Google access and a 7-minute appointment.
SRI GUNTORO
February 2, 2026 AT 05:04People are so careless with their bodies. You think your brain is a toy? You pop pills like candy and then wonder why you’re shaking? This isn’t a video game. You don’t get a respawn. If you’re on antidepressants, you should be praying every morning that you don’t make a stupid mistake. This isn’t about ‘safe’ opioids-it’s about responsibility. And most people don’t have any.
Lexi Karuzis
February 3, 2026 AT 18:53Wait… so you’re telling me the government and Big Pharma are hiding this? Of course they are. They want you sick. They want you dependent. They want you on 12 different pills so they can sell you more. They don’t want you to know that tramadol is basically a serotonin bomb. They want you to think it’s ‘just a mild painkiller.’
And what about the labs? The blood tests? Why aren’t they mandatory? Why aren’t ERs required to test for serotonin syndrome when someone comes in with fever and tremors? Because it’s cheaper to let you die than to train staff.
I’ve been saying this for years. They’re poisoning us. Slowly. Systematically. And you’re just scrolling through Reddit like it’s all normal.
Mark Alan
February 3, 2026 AT 22:47Bro. I took tramadol with Zoloft for a week. Felt like I was being electrocuted from the inside. Shaking, sweating, heart like a jackhammer. Thought I was having a panic attack. Went to urgent care. They gave me Xanax. I almost died. 😭
Now I carry a card in my wallet that says: ‘SSRI user. Do NOT give me tramadol, methadone, or dextromethorphan.’
Save your life. Print this. Laminate it. Wear it.
Amber Daugs
February 4, 2026 AT 19:11Wow. So after reading this, I realize I’ve been a terrible patient. I never asked questions. I just took what the doctor handed me. I’ve been on paroxetine for 5 years and just started oxycodone last month. I thought I was fine. But now I’m scared. I’m going to call my doctor tomorrow. I should’ve done this sooner. I’m sorry to everyone who’s lost someone to this. I didn’t know. But now I do. And I won’t be silent anymore.