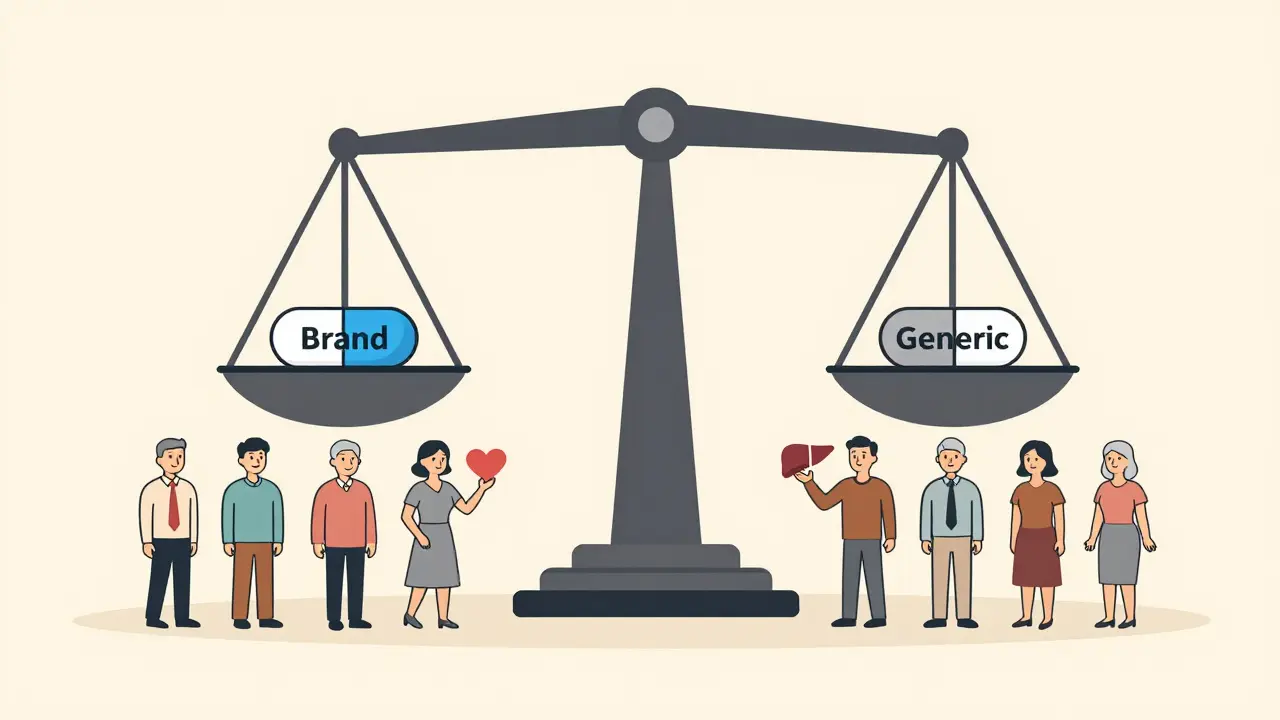
When a generic drug hits the market, it’s supposed to work just like the brand-name version. But what if the people taking it aren’t the same as the people who tested it? That’s the problem with traditional bioequivalence (BE) studies - for decades, they mostly used young, healthy men. Even today, many generic drugs are approved based on data from a group that doesn’t reflect the real users. This isn’t just a technical oversight. It can affect how well a drug works - or how safe it is - for women, older adults, and other groups. The science is catching up. Regulators are finally demanding better representation in BE studies. Here’s what you need to know about how age and sex are changing the rules.
What Bioequivalence Really Means
Bioequivalence isn’t about whether two pills look the same. It’s about whether they get into your bloodstream the same way. For a generic drug to be approved, it must deliver the same amount of active ingredient at the same speed as the original. This is measured using pharmacokinetic data - how the body absorbs, distributes, metabolizes, and clears the drug. The standard test? A crossover study where healthy volunteers take both the generic and brand-name versions, with blood samples taken over time to compare concentration curves.
For years, this was done almost exclusively in men between 18 and 30. Why? Because researchers thought men were more predictable. Their hormone levels were stable. They didn’t get pregnant. They were easier to recruit. But that logic ignored a simple fact: most drugs are taken by both men and women. And older people don’t process drugs the same way as young adults.
Why Sex Matters in Bioequivalence
Men and women don’t just differ in body size. Their bodies handle drugs differently. Women often have higher body fat percentages, lower muscle mass, slower gastric emptying, and different liver enzyme activity. These differences affect how quickly a drug is absorbed and broken down. For example, studies show that women clear certain antidepressants and painkillers slower than men. That means the same dose could lead to higher blood levels - and more side effects - in women.
One 2017 study found a generic version of a heart medication showed apparent bioinequivalence in men (79% absorption) but not in women (95% absorption). At first glance, it looked like the generic failed. But when the same study was repeated with more participants - 36 instead of 14 - the difference disappeared. The initial result wasn’t a real failure. It was a statistical fluke caused by too few women in the sample. That’s the danger of unbalanced studies: you get false alarms or miss real problems.
The U.S. Food and Drug Administration (FDA) now requires that if a drug is meant for both sexes, the BE study must include roughly equal numbers of men and women. That’s a big shift from past practice. The European Medicines Agency (EMA) says subjects “could belong to either sex” - but doesn’t require balance. That gap matters. In the U.S., sponsors now have to justify why they’d use only men - or only women - even if the drug is mostly used by one group. That’s because real-world data shows women are underrepresented. Between 2015 and 2020, only 38% of BE studies for generic drugs had between 40% and 60% female participants. The median? Just 32%. Meanwhile, 63% of people taking levothyroxine - a common thyroid drug - are women. So why are BE studies still mostly male?
Age Isn’t Just a Number
Older adults aren’t just older versions of young adults. Their kidneys and liver don’t work as fast. Their body composition changes. They often take multiple medications that interact. All of this affects how drugs behave in the body.
Regulators are starting to notice. The FDA now says if a drug is intended for elderly patients - say, over 60 - the BE study should include people in that age group. Or, if it doesn’t, the sponsor must explain why. The EMA doesn’t set a maximum age, but it does require subjects to be healthy. ANVISA in Brazil caps enrollment at age 50. That’s a problem. Many drugs for arthritis, high blood pressure, or diabetes are used mostly by people over 65. If we only test them on 30-year-olds, we’re guessing how they’ll work in the people who actually need them.
One study found that a generic version of a blood thinner showed slightly different absorption in older adults compared to younger ones - even though both groups passed the standard BE criteria. That small difference could mean a higher risk of bleeding in elderly patients. But because the study only included healthy young men, it was never caught.
Regulatory Differences Around the World
Not every agency sees this the same way. The FDA is pushing hardest for balanced representation. Their 2023 draft guidance says: “Include similar proportions of males and females.” It’s not optional anymore. The EMA still says “could belong to either sex,” leaving it up to sponsors. ANVISA requires equal male-female distribution and limits participants to ages 18-50. Health Canada allows 18-55.
These differences create headaches for drug companies. A generic drug approved in the U.S. might not meet Brazil’s rules. That means separate studies, more cost, longer timelines. Some companies stick with the lowest common denominator - testing only young men - hoping regulators won’t push back. But that’s getting riskier. The FDA is now reviewing ANDA applications more closely. If your study has 80% men and the drug is used mostly by women, you’ll get a request for more data. Or worse - a refusal.
Why It’s Hard to Get It Right
Changing the rules sounds simple. Making it happen? Not so much.
Recruiting women into clinical trials is harder. Many women juggle caregiving, work, or family responsibilities. Clinical trials often require multiple early-morning visits. Scheduling flexibility is rare. Sites report that gender-balanced studies take 40% longer to enroll. That drives up costs by 20-30%.
There’s also a mindset problem. Some researchers still believe that if a drug works in young men, it’ll work in everyone. But the data says otherwise. A 2023 University of Toronto study found that 37% of commonly tested drugs are cleared 15-22% faster in men than in women. That’s not noise. That’s biology. Ignoring it isn’t science - it’s guesswork.
And then there’s the statistical challenge. Small studies (n=12-14) are prone to outliers. One woman with unusually slow metabolism can skew results. Larger studies (n=36 or more) smooth that out. But bigger studies cost more. Many sponsors still go with the minimum required - 12 subjects - because it’s cheaper. The EMA allows that. The FDA doesn’t. And if you’re submitting to the FDA, you need to plan for more.
What’s Changing - and What’s Next
The tide is turning. The FDA’s 2023 guidance is the clearest signal yet: BE studies must reflect real patients. Industry is catching on. A 2022 survey found 68% of contract research organizations (CROs) now actively recruit women. But only 29% track sex-specific pharmacokinetic data. That’s a gap. You can’t prove equivalence if you don’t measure it separately.
Future changes are likely. The National Academies of Sciences recommended sex-specific bioequivalence criteria for narrow therapeutic index drugs - like warfarin or lithium - where small differences can be dangerous. The EMA is reviewing its 2010 guideline and may update it in 2024. More countries will likely follow the FDA’s lead.
For now, sponsors have to adapt. The best approach? Design studies with representation in mind from day one. Use stratified randomization to ensure equal sex distribution. Include older adults if the drug targets them. Run pre-specified subgroup analyses for sex and age. Don’t wait for regulators to ask. Be proactive. Because when a woman takes a generic drug and it doesn’t work like the brand, she doesn’t care about the study design. She just knows it didn’t help.
Practical Takeaways for Sponsors and Clinicians
- If the drug is used by both men and women, aim for a 50:50 split in your BE study. Don’t assume it’s fine with 70% men.
- If the drug is for older adults, include participants aged 60+. Don’t rely on data from 25-year-olds.
- Always report sex and age as baseline characteristics. Don’t bury them in a footnote.
- Run subgroup analyses for sex - even if you don’t expect differences. Sometimes the difference is in the data you didn’t look for.
- Document your rationale if you exclude a group. The FDA will ask for it.
It’s not about being politically correct. It’s about being scientifically accurate. Bioequivalence isn’t just a regulatory checkbox. It’s a promise to patients: your medicine will work like it should. That promise only holds if the people in the study look like the people taking it.
Why were bioequivalence studies historically done only on young men?
Early BE studies used young, healthy men because they were seen as more predictable. Their hormone levels were stable, they didn’t get pregnant, and recruitment was easier. Researchers believed results from this group could be generalized to everyone. But this assumption ignored biological differences in drug metabolism between sexes and age groups, leading to gaps in safety and effectiveness data for women and older adults.
Does the FDA require equal numbers of men and women in BE studies?
Yes. The FDA’s 2023 draft guidance requires that if a drug is intended for use by both sexes, applicants must include similar proportions of males and females - roughly 50:50 - unless there’s a strong scientific reason not to. This is a shift from past practice, where male-only studies were common even for drugs used mostly by women.
What age groups should be included in bioequivalence studies?
For most drugs, participants must be 18 or older. But if the drug is intended for elderly patients (typically 60+), the FDA requires inclusion of subjects in that age group - or a detailed justification for exclusion. The EMA allows adults 18+, while ANVISA limits enrollment to 18-50. Age restrictions vary, but the trend is toward including populations that match the drug’s real-world users.
Can a BE study done in young men be used to approve a drug for older women?
Not reliably. While regulators allow extrapolation in some cases, it requires strong scientific justification. Older adults and women metabolize drugs differently due to changes in liver and kidney function, body composition, and hormone levels. A study in young men may miss key differences that affect safety or effectiveness in older women. The FDA now expects sponsors to test in the target population whenever possible.
Are there real-world examples where sex differences caused problems with generic drugs?
Yes. A 2017 study found a generic heart medication appeared bioinequivalent in men (79% absorption) but not in women (95%). The initial result suggested failure - but when the study was repeated with a larger sample size (n=36), the difference vanished. The problem wasn’t the drug - it was the small, unbalanced sample. Without enough women, statistical noise looked like a real failure. This shows why balanced representation matters.



Neil Ellis
January 22, 2026 AT 03:35Finally someone’s talking about this like it matters. I’ve been prescribing generics for years and noticed women on the same dose as men would either crash or feel nothing. Turns out, it’s not them - it’s the damn studies. We’ve been treating biology like a glitch, not a feature. Time to fix it.
Lana Kabulova
January 23, 2026 AT 13:40So… let me get this straight: we’ve been approving drugs based on data from 18–30-year-old men, even for medications taken by 70% women over 65? And you’re surprised some people say the generic doesn’t work? That’s not science. That’s negligence wrapped in a lab coat. The FDA’s 2023 guidance is a start - but why did it take this long? And why are we still using n=12 studies?!
Rob Sims
January 25, 2026 AT 03:37Oh wow. A whole article about how men aren’t the default human. Groundbreaking. Next you’ll tell us water is wet and gravity exists. Look, if you want to overcomplicate drug trials, go ahead. But let’s be real - most of these drugs are fine. The people who complain about generics not working? Usually just want the brand name because it’s ‘better.’ Spoiler: it’s not.
Kenji Gaerlan
January 26, 2026 AT 09:13bro why are we even doing this? i mean like… if the pill looks the same and costs less, who cares if a 68 year old woman metabolizes it slower? she’s probably on 12 other meds anyway. just give her the generic and move on. stop overthinking it.
Margaret Khaemba
January 26, 2026 AT 19:19My grandma takes levothyroxine and swears the generic gives her heart palpitations. The brand? Perfect. I always thought it was placebo… until I read this. Now I get it. It’s not in her head - it’s in the data. We need to stop pretending biology is optional. Also, can we PLEASE stop requiring 8am blood draws? My cousin missed 3 visits because she had to drop her kid off at school first. Flexibility isn’t a perk - it’s equity.
Malik Ronquillo
January 27, 2026 AT 04:25Y’all act like this is some new revelation. Nah. This has been obvious since the 90s. But nobody wanted to pay for bigger studies. So we got lazy. Now the FDA’s saying ‘nope’ and suddenly it’s a crisis? Wake up. The science was always there. We just chose to ignore it because it was cheaper. And now? Now we’re paying for it - in side effects, ER visits, and lost trust.
Brenda King
January 27, 2026 AT 07:21Thank you for writing this. I’ve been in pharma for 15 years and watched this happen over and over. We’d get results back, see a 15% difference in women, and the response was always ‘oh, that’s within variability.’ No. It’s not. It’s biology. We need to start reporting sex-specific AUC and Cmax. Not just burying it in appendix B. And yes - we need older adults. My dad took a blood thinner and almost bled out because the study didn’t include anyone over 50. He’s not a lab rat. He’s a patient.
Keith Helm
January 27, 2026 AT 13:15Regulatory divergence is inefficient. Harmonization is required. The EMA’s permissive stance undermines FDA efforts. Global supply chains demand uniform standards. Inconsistent requirements increase cost and delay access. A unified framework is not optional.
Daphne Mallari - Tolentino
January 29, 2026 AT 04:14It is rather regrettable that the scientific community has, for so long, indulged in the anthropocentric fallacy of assuming homogeneity across biological substrata. The reductionist paradigm of using young, male, healthy subjects as universal proxies is not merely methodologically flawed - it is epistemologically indefensible. One must question the very epistemic authority of such data when applied to heterogeneous populations. The FDA’s guidance, while tardy, is at least a step toward epistemic integrity.
Alec Amiri
January 30, 2026 AT 03:06Let’s be real - this is just woke science. You want to test on every demographic? Cool. Now tell me how you’re gonna pay for it. You think drug prices won’t go up? You think insurance won’t drop coverage? You think patients won’t suffer because generics are too expensive to make? This isn’t progress - it’s a money pit wrapped in virtue signaling.
Patrick Roth
January 30, 2026 AT 12:48Actually, you’re all wrong. The real issue is that we’re still using blood draws as the gold standard. We should be using saliva or wearable sensors. Also, why are we assuming sex and age are the only variables? What about gut microbiome? Ethnicity? Sleep patterns? You’re all missing the forest for the trees. And no, I didn’t read the whole article - but I know more than you do.