Not all bad reactions to medicine are allergies
Many people say they’re "allergic" to a medication because it made them feel sick. But if you got nauseous after taking ibuprofen, or felt dizzy after starting a new blood pressure pill, that’s not an allergy. It’s a side effect. And confusing the two can put your health at risk.
Every year, millions of people avoid important medications because they think they’re allergic - but they’re not. The CDC says only 1% of people who claim a penicillin allergy actually have one. The other 99%? They had a side effect, or maybe an intolerance. And because they were mislabeled, they got weaker, more expensive, or riskier drugs instead. That’s not just inconvenient - it’s dangerous.
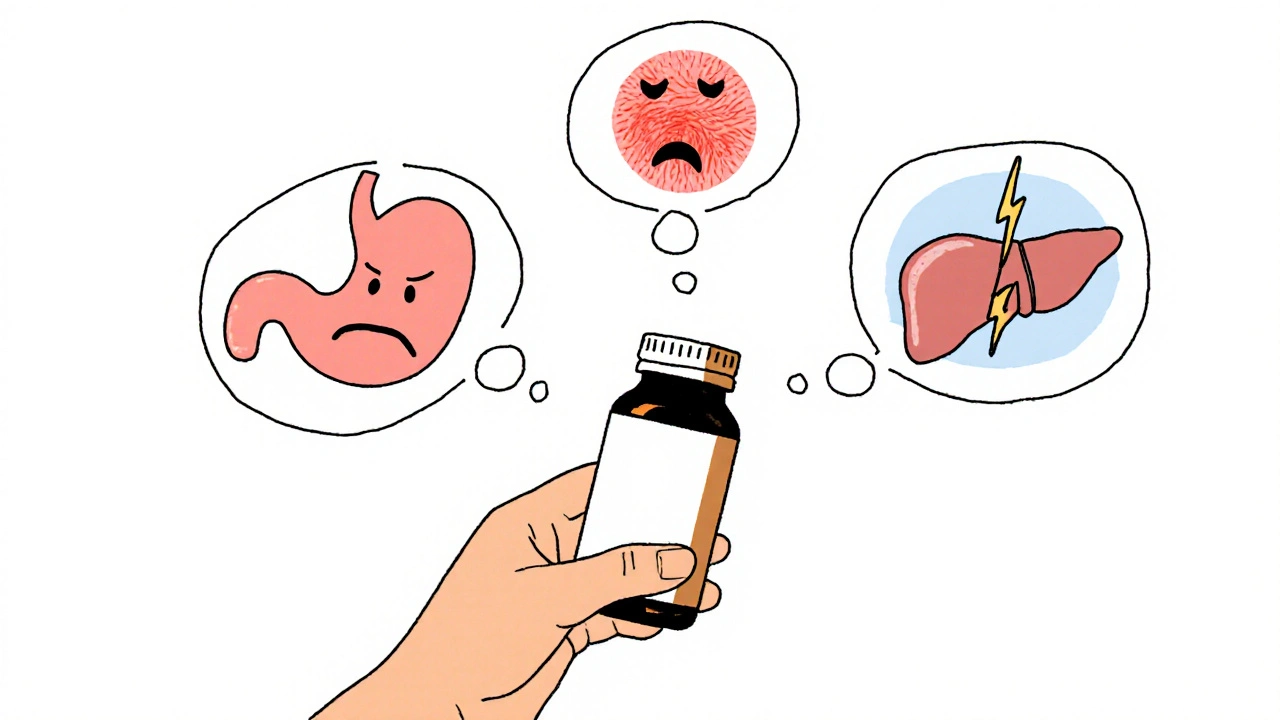
What’s a side effect?
A side effect is a known, predictable reaction to how a drug works in your body. It’s not your immune system reacting. It’s the drug doing exactly what it’s supposed to do - just in a way that causes discomfort.
For example:
- NSAIDs like ibuprofen can cause stomach upset in 25-30% of users because they interfere with protective stomach lining chemicals.
- SSRIs like sertraline often cause dizziness or sleepiness in about 15% of people, because they change brain chemistry.
- First-generation antihistamines like diphenhydramine make you sleepy in up to 40% of users - that’s the whole point of the drug, just not the one you wanted.
These reactions are dose-dependent. Take more, and the effect gets stronger. Take less, or take it with food, and it often gets better. Many side effects fade after a few days as your body adjusts. If they don’t, your doctor can lower the dose, switch the timing, or add another medicine to counteract it.
Side effects are listed in the drug’s package insert. They’re not surprises. They’re expected. And they’re not life-threatening.
What’s a true allergic reaction?
An allergic reaction means your immune system has mistaken the drug for a threat - like a virus or pollen - and is attacking it. This is rare. Only 5-10% of all bad reactions to medicine are true allergies.
True drug allergies show up fast - usually within minutes to an hour after taking the drug. And they involve your body’s emergency response system:
- Hives (red, itchy welts on the skin)
- Swelling of the lips, tongue, or throat (angioedema)
- Wheezing, chest tightness, trouble breathing
- Dizziness, rapid pulse, dropping blood pressure (signs of anaphylaxis)
Anaphylaxis is medical emergency. It can kill within minutes. If you’ve ever needed epinephrine (an EpiPen) after taking a medicine, you likely had a true allergy.
There’s also a delayed type of allergic reaction - like DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms). It shows up days or weeks later with rash, fever, swollen glands, and organ damage. It’s rare but deadly - up to 10% of people with DRESS don’t survive.
Unlike side effects, allergies don’t get better with lower doses. They get worse with each exposure. Once you’ve had one, you must avoid that drug - and sometimes others like it - for life.
What’s drug intolerance?
Intolerance is the messy middle ground. It’s not an allergy - your immune system isn’t involved. But it’s not just a typical side effect either. It’s when your body reacts badly to a drug at normal doses, while most people handle it fine.
Examples:
- Some people get severe asthma attacks or nasal congestion from aspirin or ibuprofen - even though they’ve never had hives or swelling. This is called aspirin-exacerbated respiratory disease (AERD). It affects about 7% of adults with asthma.
- Codeine can cause violent vomiting in people with a genetic variation that turns it into morphine too quickly. This isn’t an allergy - it’s a metabolic quirk.
- Some people get diarrhea from metformin even at the lowest dose, while others take it for years with no issues.
Intolerance is often genetic. It’s tied to how your liver processes drugs or how sensitive your body is to certain chemicals. You might tolerate one drug in a class but not another. For example, someone with AERD might react to ibuprofen but not celecoxib.
Doctors diagnose intolerance by ruling out allergy and side effect. If the reaction happens at normal doses, doesn’t involve hives or swelling, and isn’t typical for the drug, it’s likely intolerance.
Why does it matter?
Mixing up these reactions isn’t just a labeling mistake - it changes your treatment and your risk.
If you’re wrongly labeled as allergic to penicillin, you’re more likely to get stronger antibiotics like vancomycin or clindamycin. Those drugs:
- Cost 30% more
- Are less effective for some infections
- Increase your chance of getting a deadly gut infection called C. diff by 30%
- Raise your risk of MRSA by 50%
One study found people with mislabeled penicillin allergies had hospital stays 1.2 days longer on average. That’s $2,500 extra in costs per person - and it’s all because someone thought diarrhea meant allergy.
On the flip side, if you ignore a real allergy and take the drug again, you could go into anaphylaxis. That’s not a risk you can afford to gamble with.
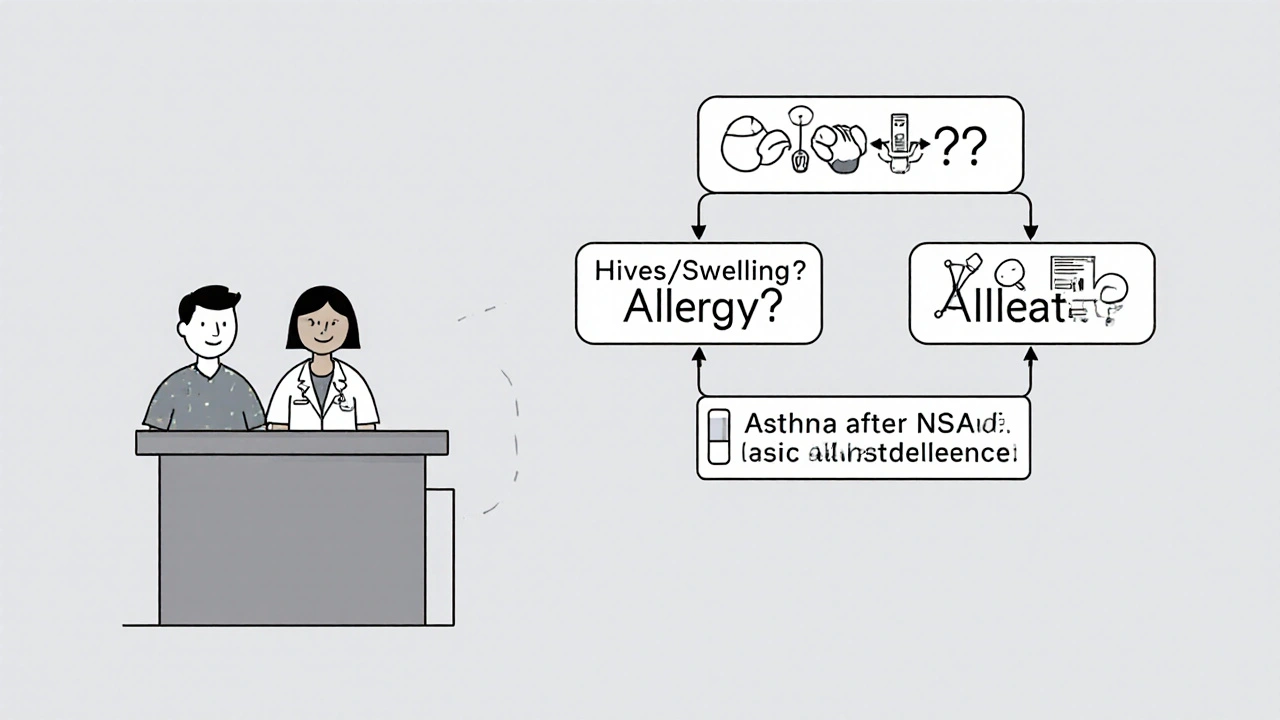
How to tell them apart
Ask yourself these questions:
- When did it happen? Within 1 hour? Could be allergy. Took days? Could be DRESS or intolerance. Took hours? Probably side effect.
- What happened? Hives, swelling, trouble breathing? That’s allergy. Nausea, headache, drowsiness? Side effect. Asthma flare-up after NSAIDs? Likely intolerance.
- Did it happen every time? Only once? Might be a fluke. Happened every time? More likely to be intolerance or allergy.
- Did you need emergency treatment? Epinephrine? Hospitalization? That’s a red flag for allergy.
Don’t rely on memory. Write down:
- The name of the drug
- When you took it
- What symptoms you had
- How long they lasted
- What you did to treat them
Bring this to your doctor. If you’re unsure, ask for a referral to an allergist. Skin tests and oral challenges are safe, accurate, and can clear up confusion in one visit.
What to do if you think you’re allergic
Stop taking the drug immediately if you have signs of anaphylaxis - and call 999. That’s non-negotiable.
If you’re not sure, don’t assume. Don’t tell your doctor, "I’m allergic to penicillin." Say this instead:
"I had [symptoms] after taking [drug] on [date]. It was [nausea/hives/swelling/breathing trouble]. I didn’t need epinephrine. I’ve never had it again. I’d like to know if this was a true allergy or something else. Can you refer me to an allergist?"
Many hospitals now have drug allergy clinics. The CDC recommends testing for anyone with a penicillin allergy label. It’s quick, safe, and often covered by insurance.
Getting tested doesn’t mean you’ll lose your label. It means you’ll know the truth - and get better care.
What your doctor should do
Doctors are being trained to stop writing "allergy" on charts for nausea, dizziness, or mild rashes. The American Medical Association now says:
- Use "side effect" for predictable, non-immune reactions
- Use "intolerance" for exaggerated reactions at normal doses
- Use "allergy" only when immune system involvement is confirmed
Electronic health records now pop up warnings if you type "allergy" for a common side effect. That’s because the system knows: mislabeling costs lives.
If your doctor dismisses your concern, ask: "Could this be something other than an allergy? Can we check?" You have the right to know exactly what happened - and why.
What’s changing right now
Things are improving. In 2023, the FDA launched a program using AI to scan millions of medical records to catch mislabeled allergies. The NIH is funding a 15-minute penicillin test you could get in your doctor’s office. And clinical trials like PEN-FAST are proving that simple questions can safely identify who doesn’t need testing at all.
Genetic testing is also becoming more common. For example, before giving HIV patients abacavir, doctors now test for the HLA-B*57:01 gene. If you have it, you’re at high risk of a severe reaction - so you’re given a different drug. That’s precision medicine. And it’s saving lives.
Bottom line
Not every bad reaction is an allergy. Most aren’t. But if you don’t know the difference, you might avoid life-saving drugs - or worse, take one that could kill you.
If you’ve ever had a reaction to medicine, don’t just label it. Understand it. Write it down. Talk to your doctor. Ask for testing if it was serious or confusing.
Knowing the difference between side effect, intolerance, and allergy isn’t just about labels. It’s about getting the right treatment, avoiding unnecessary risks, and living healthier - without fear of the medicine you need.



Scott Macfadyen
November 17, 2025 AT 21:24Chloe Sevigny
November 19, 2025 AT 09:23Denise Cauchon
November 19, 2025 AT 14:43Andrea Johnston
November 20, 2025 AT 02:11Victoria Malloy
November 21, 2025 AT 01:43Alex Czartoryski
November 22, 2025 AT 05:24Gizela Cardoso
November 24, 2025 AT 05:15Ancel Fortuin
November 26, 2025 AT 04:43Hannah Blower
November 26, 2025 AT 16:26Gregory Gonzalez
November 27, 2025 AT 21:59Ronald Stenger
November 29, 2025 AT 11:55Samkelo Bodwana
November 30, 2025 AT 03:49