Medication Interaction Risk Checker
Check for Dangerous Medication Interactions
This tool helps you identify potentially dangerous medication combinations that can cause rhabdomyolysis, a serious muscle breakdown condition. Based on data from the article, this checker focuses on high-risk interactions involving statins and other common drugs.
When you take a statin for cholesterol or colchicine for gout, you don’t expect your muscles to start breaking down. But when two common medications mix, they can trigger a silent, dangerous process called rhabdomyolysis-a condition where muscle cells rupture and spill their contents into your bloodstream. This isn’t rare. It’s not just a footnote in a drug label. It’s a real emergency that sends over 27,000 Americans to the hospital every year, many of them older adults on multiple prescriptions.
What Exactly Is Rhabdomyolysis?
Rhabdomyolysis happens when skeletal muscle tissue breaks down rapidly. The inside of muscle cells-things like creatine kinase (CK), potassium, phosphate, and myoglobin-leak out. Myoglobin is especially dangerous. When it floods the kidneys, it clogs the tiny filters and can cause acute kidney failure. Up to half of people with severe rhabdomyolysis end up needing dialysis.The classic signs-muscle pain, weakness, and dark urine-are only present in about half the cases. Many people don’t realize anything’s wrong until they’re already in trouble. Some feel nausea, fever, or abdominal pain. Others just feel unusually tired. By the time they go to the ER, their CK levels might be over 50,000 U/L. Normal is under 200. That’s not a typo.
Medications Are the Leading Cause
About 7-10% of all rhabdomyolysis cases come from drugs. And most of those? They’re not from one drug alone. They’re from interactions.Statins-like atorvastatin (Lipitor) and simvastatin (Zocor)-are responsible for nearly two-thirds of all drug-induced cases. But here’s the catch: when you take a statin with certain other drugs, your risk doesn’t just go up. It explodes.
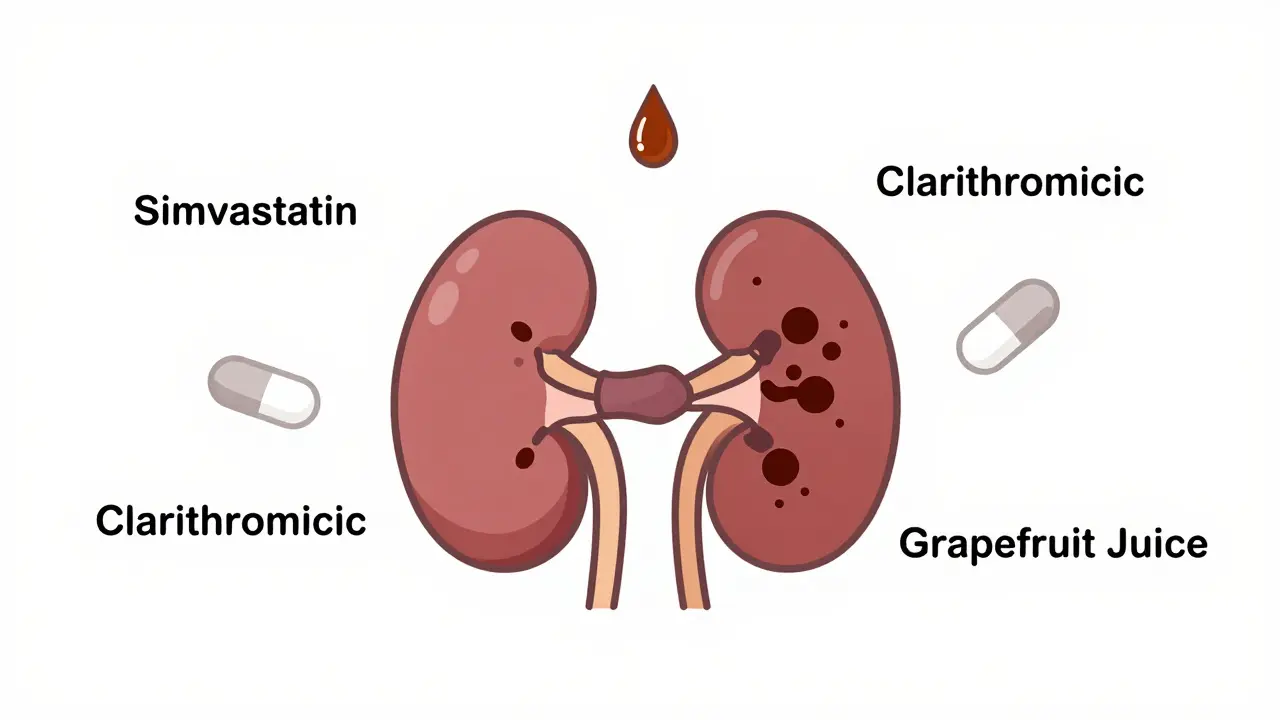
For example, combining simvastatin with the antibiotic erythromycin increases your risk by almost 19 times. Why? Because both drugs are processed by the same liver enzyme, CYP3A4. When one blocks it, the other builds up to toxic levels in your blood. Same thing happens with azole antifungals like itraconazole, or the common heartburn drug clarithromycin. A 2021 FDA review found that 89% of fatal statin-related rhabdomyolysis cases involved one of these combinations-even though they made up just 12% of all statin prescriptions.
It’s not just statins. Colchicine, used for gout, is safe on its own. But when paired with clarithromycin or grapefruit juice, the risk jumps 14-fold. One patient reported his urine turned cola-colored within 48 hours after adding clarithromycin to his regimen. His CK hit 28,500 U/L. He needed hospitalization.
Who’s Most at Risk?
Some people are far more likely to develop this than others. Age matters. If you’re over 65, your risk is more than three times higher. Women have a 70% greater chance than men. And if you have reduced kidney function-even mild-you’re nearly five times more vulnerable.But the biggest red flag? Polypharmacy. Taking five or more medications? That raises your risk by over 17 times. It’s not just the drugs themselves. It’s how they interact. A 72-year-old woman on simvastatin, amiodarone, leflunomide, and a proton pump inhibitor is sitting on a ticking time bomb. Her liver can’t keep up. Her kidneys are already strained. One new prescription-maybe an antifungal for a toenail infection-and boom.
Genetics play a role too. About 15% of Europeans carry a gene variant called SLCO1B1*5. It makes their bodies absorb statins too efficiently. If you have this variant and take simvastatin, your risk of muscle damage is 4.5 times higher. Most doctors don’t test for it. They shouldn’t have to. The labels should warn everyone.
Deadly Combinations You Might Not Know About
Here are some of the most dangerous pairings, backed by real cases and data:- Simvastatin + Erythromycin or Clarithromycin - 18-19x higher risk
- Simvastatin + Gemfibrozil - 15-20x higher risk
- Colchicine + Clarithromycin - 14.2x higher risk
- Statin + Itraconazole (antifungal) - 12x higher risk
- Erlotinib (cancer drug) + Simvastatin - CK levels over 20,000 U/L reported within 72 hours
- Propofol (anesthesia) + prolonged infusion - 68% mortality if rhabdomyolysis develops
Leflunomide, a drug for rheumatoid arthritis, is rare but brutal. It has a half-life of two weeks. Once it starts breaking down muscle, your body can’t flush it out fast enough. In two documented cases, patients needed plasma exchange-literally filtering their blood-to survive.
How Doctors Miss It
Patients often report muscle aches early. But too often, doctors dismiss it as "just aging" or "exercise soreness." A 2022 Reddit thread with 147 reported cases showed that 92% of patients said their provider didn’t recognize the warning signs.One man started simvastatin after a heart attack. Two weeks later, his shoulders and thighs ached. He mentioned it at his follow-up. His doctor told him to "take it easy." Three days later, he couldn’t walk. His CK was 42,000. He needed dialysis.
It’s not just patient silence. It’s system failure. Many electronic health records don’t flag high-risk combinations unless the drug names are typed in exactly right. Grapefruit juice? Not in the system. Over-the-counter antifungals? Not tracked. The tools exist-but they’re not used well.
What to Do If You Suspect Rhabdomyolysis
If you’re on any of these medications and suddenly feel:- Severe muscle pain or weakness
- Dark, tea- or cola-colored urine
- Unexplained fatigue or nausea
Stop the medication immediately. Call your doctor. Go to the ER. Don’t wait. This isn’t something you can treat at home.
Emergency treatment is straightforward but urgent:
- Stop the offending drug(s)
- Start aggressive IV fluids-3 liters in the first 6 hours, then 1.5 liters per hour
- Add sodium bicarbonate to keep your urine pH above 6.5 (this stops myoglobin from clumping in your kidneys)
- Monitor potassium, calcium, and kidney function hourly
Most people recover if treated fast. But if kidney failure sets in, recovery takes months. Some never fully regain their strength.
Long-Term Effects
Even if you survive, rhabdomyolysis can leave lasting damage. A 10-year Mayo Clinic study found that 44% of survivors still had muscle weakness six months later. Those who needed dialysis took nearly three times longer to recover than those who didn’t.And here’s the quiet crisis: as people live longer and take more medications, this problem is growing. The JAMA Internal Medicine study from 2022 predicts rhabdomyolysis cases will rise by over 8% per year through 2030. Without better drug safety systems, we’re heading for a wave of preventable kidney injuries.
How to Protect Yourself
You can’t avoid all medications. But you can reduce your risk:- Know your meds. Keep a written list of everything you take-including supplements and OTC drugs.
- Ask your pharmacist: "Can this interact with my other drugs?" Don’t assume they know your full list.
- If you’re over 65 or have kidney issues, ask if your statin dose is the lowest possible.
- Never take grapefruit juice with statins, colchicine, or certain blood pressure meds.
- Report muscle pain early. Don’t wait for dark urine.
- Ask if you need a CK test if you start a new drug and feel unwell.
The FDA and EMA have issued warnings. But warnings on a label don’t save lives. Awareness does. Communication does. If you’re taking more than three medications, have a conversation-not just with your doctor, but with your pharmacist. Ask: "Could any of these hurt my muscles?"
Because rhabdomyolysis doesn’t come with a siren. It comes with a whisper. And if you don’t listen, it can cost you your kidneys-or your life.
Can rhabdomyolysis happen from just one medication?
Yes, but it’s rare. Most cases are triggered by drug interactions. Statins alone can cause rhabdomyolysis, especially at high doses or in people with kidney disease, but the risk jumps dramatically when combined with other drugs like antibiotics, antifungals, or fibrates. About 60% of drug-induced cases involve a combination.
What are the first signs of rhabdomyolysis?
The classic signs are muscle pain, weakness, and dark urine-but only about half of patients show all three. Early warning signs include unusual fatigue, unexplained muscle soreness, nausea, or fever. If you’re on a statin or similar drug and feel like you’ve been hit by a truck after doing nothing, don’t ignore it. Dark urine is a red flag-treat it like a medical emergency.
Is rhabdomyolysis always permanent?
No, if caught early, most people recover fully. But if kidney damage occurs, recovery takes longer-and some never regain full muscle strength. Studies show 44% of survivors still have weakness after six months. Those needing dialysis may take over six months to recover. The key is speed: the sooner treatment starts, the better the outcome.
Which statins are safest regarding muscle damage?
Pravastatin and rosuvastatin are less likely to cause muscle problems because they’re not processed by the CYP3A4 enzyme. Simvastatin and atorvastatin carry the highest risk, especially when combined with other drugs. If you’re on a high-risk statin and take multiple medications, ask your doctor if switching to pravastatin or rosuvastatin is an option.
Can I take over-the-counter pain relievers if I’m on a statin?
Acetaminophen (Tylenol) is generally safe. Avoid NSAIDs like ibuprofen or naproxen if you have kidney issues or are dehydrated-they can add stress to your kidneys when combined with muscle breakdown. Always check with your pharmacist before mixing any OTC drug with your prescription meds.
Should I get genetic testing before taking statins?
Not routinely. Testing for the SLCO1B1*5 gene is expensive and not widely available. But if you’ve had muscle pain on statins before, or if you’re on multiple interacting drugs, it might be worth discussing. The real solution is better drug interaction alerts in electronic health records-not genetic tests for everyone.
How can I check if my meds interact?
Use a reliable drug interaction checker like Medscape or Micromedex, but don’t rely on apps alone. Bring your full list-prescriptions, supplements, OTCs-to your pharmacist. They’re trained to spot dangerous combinations. If your doctor doesn’t ask about everything you take, ask them: "Could any of these hurt my muscles?"




Stephen Craig
January 4, 2026 AT 22:29It’s terrifying how quietly this kills people. No siren, no warning-just fatigue and dark urine, and suddenly you’re in dialysis. We treat meds like candy, but the body doesn’t care about prescriptions-it just reacts.
Connor Hale
January 6, 2026 AT 16:50Doctors aren’t villains. They’re drowning in charts, alerts, and time limits. The system’s broken, not the individuals. We need better EHR integration-not just more warnings, but context-aware flags that actually pop up when a 72-year-old on five meds gets a new script.
bob bob
January 7, 2026 AT 23:56My uncle had this happen after he started clarithromycin for a sinus thing. He was on simvastatin too. Didn’t even know grapefruit juice was a problem. He’s fine now, but he’ll never take meds without checking with his pharmacist first. Seriously, talk to them. They’re the real MVPs.
Abhishek Mondal
January 9, 2026 AT 05:54Let’s be clear: this isn’t about drug interactions-it’s about the abdication of clinical responsibility. The FDA issues warnings, but they’re buried in 200-page PDFs. Meanwhile, pharmacists are pressured to fill scripts faster than they can read them. The real culprit? Profit-driven healthcare systems that treat patients as data points-not humans. And yes, I’m aware this is an oversimplification-but so is the entire medical-industrial complex.
Terri Gladden
January 10, 2026 AT 07:50OMG I JUST REALIZED I TOOK GINGER TEA WITH MY STAIN AND CLARITHROMYCIN??!! I THINK IM GONNA DIE??!!
Jennifer Glass
January 10, 2026 AT 23:12I’ve been on rosuvastatin for years and never had issues, but after my doctor added amiodarone, I started feeling like I’d run a marathon just walking to the fridge. I asked for a CK test-and it was over 18,000. They switched me to pravastatin immediately. No drama. Just science. If you’re on more than three meds, don’t wait for symptoms. Ask for a baseline CK. It’s a five-minute blood test.
Joseph Snow
January 12, 2026 AT 11:36Let’s not pretend this is accidental. The pharmaceutical industry knows these interactions are deadly. They market statins like miracle drugs while burying the risks in fine print. The FDA? Complicit. The doctors? Complicit. This isn’t negligence-it’s systemic malice disguised as medicine. Wake up. You’re being used as a test subject.
melissa cucic
January 13, 2026 AT 05:51Thank you for writing this with such precision. The statistics are horrifying-but what’s more disturbing is how rarely these combinations are flagged during medication reconciliation. I work in a hospital pharmacy, and we still see patients on simvastatin + clarithromycin, even though the guidelines have been clear since 2018. The EHRs don’t alert unless the exact brand names are entered. Generic versions? Forgotten. Grapefruit juice? Not in the system. We’re not failing patients because we’re careless-we’re failing them because the tools we’re given are designed for efficiency, not safety.
Jacob Milano
January 13, 2026 AT 14:34This hits different when you’ve seen someone you love turn into a ghost because their muscles just… gave out. I watched my dad go from hiking every weekend to needing a walker because his legs wouldn’t hold him. He didn’t even know grapefruit juice was a problem. Now I carry a laminated card in my wallet with every med I take-and I quiz my pharmacist every time I pick up a new script. Don’t wait for the dark urine. If your body feels wrong, it’s not just ‘getting old.’ It’s screaming.
saurabh singh
January 13, 2026 AT 21:17Bro, in India we don’t even know what statins are half the time-but when we do, we take them with chai and no questions. This post is a wake-up call. My aunt had this happen after she took an OTC antifungal for her foot fungus. She didn’t even tell her doctor. Please, if you’re taking meds, write them down. Show your pharmacist. Ask the dumb questions. Your muscles will thank you.
Allen Ye
January 14, 2026 AT 18:24The fundamental flaw in modern pharmacology is the assumption that biological systems operate with linear causality. Rhabdomyolysis is not merely an interaction between two drugs-it is the emergent consequence of a complex, nonlinear physiological network disrupted by pharmacokinetic interference, genetic polymorphisms, age-related decline in hepatic and renal clearance, and the absence of systemic safety architecture. The current paradigm of individualized drug labeling ignores the systemic nature of polypharmacy. We are not treating patients-we are treating isolated variables in a dynamic system that demands holistic modeling. Until regulatory agencies and clinical informatics evolve beyond static drug interaction databases and embrace dynamic, patient-specific metabolic simulations, this epidemic will persist. The data is clear. The solutions exist. The will to implement them does not.
mark etang
January 16, 2026 AT 01:31It is imperative that all stakeholders within the healthcare ecosystem-clinicians, pharmacists, regulatory bodies, and patients-adhere to evidence-based protocols in the administration of pharmacological agents. The incidence of drug-induced rhabdomyolysis is a direct consequence of noncompliance with established clinical guidelines and insufficient interdisciplinary communication. It is the responsibility of each individual to ensure that their medication regimen is reviewed by a qualified pharmacist prior to initiation of any new agent. Failure to do so constitutes a breach of personal health stewardship.