Switching from a brand-name drug to a generic version is common - it saves money, and in most cases, it works just as well. But for some people, the switch doesn’t go smoothly. Maybe your seizures returned. Maybe your blood pressure spiked. Or maybe you just feel off, even though your doctor says the generic is "the same." You’re not imagining it. And you’re not alone.
Why Some People Notice a Difference After a Generic Switch
The FDA says generics must be bioequivalent to the brand-name version. That means the active ingredient must deliver the same amount of medicine into your bloodstream within the same time frame - usually within 80% to 125% of the brand’s levels. Sounds tight, right? But here’s the catch: that 25% window allows for real differences in how your body responds. For drugs with a narrow therapeutic index - like warfarin, levothyroxine, or seizure meds - even small changes in blood levels can cause problems. One study found that 23.4% of patients switched from brand to generic levothyroxine had thyroid hormone levels jump out of the safe range within six months. That’s more than one in five people. Meanwhile, only 8.2% of those who stayed on the brand had the same issue. And it’s not just about the active ingredient. Generics can have different fillers, dyes, or coatings. For someone with a sensitivity - say, to lactose or a specific dye - that change can trigger side effects or make them stop taking the medicine altogether. In one survey, 83% of pharmacists reported patients quitting generics because they felt the drug wasn’t working as well, especially for psychiatric or epilepsy meds.What to Track After a Generic Switch
You can’t just wait and hope things work out. You need to track specific signs. Here’s what matters most:- Lab results: For drugs like warfarin (INR levels), levothyroxine (TSH), or digoxin (blood concentration), get your numbers checked within 7 to 14 days after switching. Then again at 30 and 90 days. A change of 15% or more from your baseline is a red flag.
- Symptoms: Did your seizures get worse? Are you dizzy, tired, or having chest pain? Write them down. Don’t wait for your next appointment. If you notice a pattern, call your doctor.
- Medication gaps: If you stop taking the generic for more than 90 days, that’s a strong signal something’s wrong. Studies show this is one of the best ways to spot problems - it’s not just about side effects, it’s about whether you trust the medicine enough to keep taking it.
- Hospital visits: A spike in ER trips, urgent care visits, or hospital stays after the switch? That’s not coincidence. For digoxin, switching to generic was linked to a 34.7% rise in hospitalizations for toxicity.
- How you feel: Your experience matters. If you feel worse, even if labs look fine, speak up. The FDA itself says patient-reported outcomes are part of the safety picture.
Which Medications Need the Most Attention
Not all generics are created equal. Some are safe to switch without worry. Others? Not so much. High-risk drugs (Narrow Therapeutic Index):- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin, carbamazepine, valproate (seizure meds)
- Digoxin (heart medication)
- Lithium (mood stabilizer)
- Cyclosporine (immunosuppressant)
- Lisinopril (blood pressure)
- Atorvastatin (cholesterol)
- Metformin (diabetes)
- Fluoxetine (antidepressant)
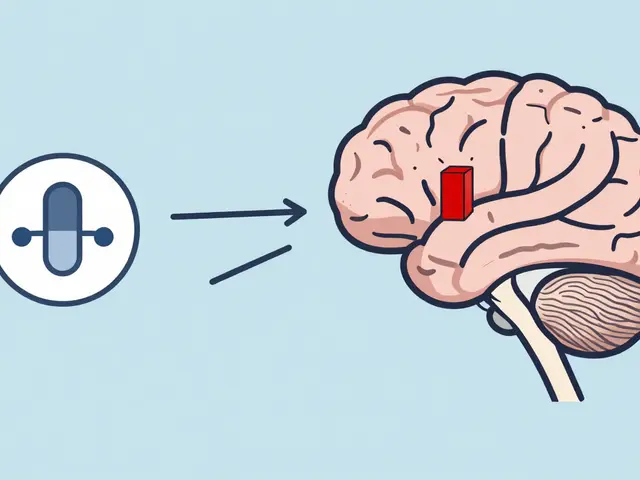
How to Monitor Effectiveness - Step by Step
Here’s a simple, practical plan to follow after your doctor switches you to a generic:- Before the switch: Write down your current lab values, symptoms, and daily routine. Take a photo of your prescription bottle. This is your baseline.
- Day 1-7: Call your pharmacist. Ask: "Is this the same generic you’ve used before?" Some pharmacies switch between manufacturers without telling you. That can cause problems too.
- Day 7-14: Get your key lab test done. For warfarin, check INR. For thyroid meds, check TSH. For epilepsy, check drug levels if possible.
- Day 30: Ask yourself: "Do I feel different?" Write down any new side effects or changes in how you function. Call your doctor if anything’s off.
- Day 90: Repeat the lab test. If your numbers are stable and you feel okay, you’re likely fine. If not, talk to your doctor about switching back.
What to Do If the Generic Isn’t Working
If you notice problems, don’t just quit the medicine. Don’t wait. Act.- Call your doctor. Say: "I switched to the generic and I’m having [symptoms]. Can we check my levels?"
- Ask for a copy of your lab results. Compare them to your pre-switch numbers.
- If labs are abnormal or symptoms persist, ask if you can go back to the brand-name version. You have the right to request it.
- If your insurance won’t cover the brand, ask your doctor to write a letter of medical necessity. Many insurers approve it if you’ve had a documented issue.
- If you’re on Medicare Part D, you may qualify for a medication therapy management (MTM) session. These are free consultations with a pharmacist to review all your meds - use it.
The Bigger Picture: Why Tracking Matters
Generic drugs save the U.S. healthcare system over $300 billion a year. That’s huge. But if people stop taking their meds because they feel worse - or end up in the hospital - the cost goes back up. The FDA is starting to pay attention. Starting in 2024, every new generic for a narrow therapeutic index drug must include post-market studies to track real-world outcomes. New tools are coming too: AI models that predict who’s at risk, EHR alerts that flag abnormal lab trends, and even an FDA-approved app for patients to report side effects in real time. But until those systems are everywhere, you’re your own best advocate. No one else is watching your numbers, your symptoms, your life. If you feel different after a switch - track it. Document it. Speak up.When to Ask for the Brand Again
You don’t have to settle for a generic that doesn’t work. Here’s when to push back:- Your lab values changed significantly (15% or more) after switching.
- You had a medical event - seizure, fall, heart issue - that didn’t happen before.
- You stopped taking the medicine for more than 90 days because you didn’t trust it.
- Your doctor didn’t warn you about the switch, and you’re now having side effects.
- You’re on a drug with an "BX" rating in the FDA Orange Book.
Are generic drugs really the same as brand-name drugs?
For most drugs, yes - generics work just as well. But for medications with a narrow therapeutic index - like warfarin, thyroid hormone, or seizure drugs - even small differences in how the body absorbs the medicine can matter. The FDA requires generics to be bioequivalent, but that allows for up to a 25% variation in blood levels. For some people, that’s enough to cause problems.
How long should I wait before deciding if the generic is working?
For most drugs, give it 30 to 90 days. But for high-risk medications like warfarin or levothyroxine, check lab results within 7 to 14 days. If your numbers are off or you feel worse, don’t wait - call your doctor. Waiting too long can lead to serious complications.
Can I ask my doctor to keep me on the brand-name drug?
Yes, absolutely. You have the right to request the brand-name version, especially if you’ve had a bad reaction to the generic. Your doctor can write a letter of medical necessity to your insurance. Many insurers will approve it if you’ve documented symptoms or lab changes after switching.
Why do some pharmacists switch between different generic brands without telling me?
Pharmacies often switch generic manufacturers to get the lowest price. But different manufacturers can use different fillers or manufacturing methods - and that can affect how the drug works for you. Always ask your pharmacist: "Is this the same generic I got last time?" If it’s different, ask if you can stick with the one that worked before.
What should I do if I think my generic medication isn’t working?
Don’t stop taking it. Don’t assume it’s "all in your head." Track your symptoms and lab results. Call your doctor and say: "I switched to the generic and I’m having [specific issue]. Can we check my levels?" If your numbers are abnormal or symptoms persist, ask to switch back. You’re not being difficult - you’re protecting your health.



Elizabeth Cannon
January 24, 2026 AT 03:32Luke Davidson
January 25, 2026 AT 06:46Marlon Mentolaroc
January 25, 2026 AT 12:19Dolores Rider
January 25, 2026 AT 18:12Sawyer Vitela
January 26, 2026 AT 14:02Viola Li
January 27, 2026 AT 05:05Jenna Allison
January 29, 2026 AT 04:24venkatesh karumanchi
January 30, 2026 AT 18:27Jamie Hooper
February 1, 2026 AT 15:23Vatsal Patel
February 2, 2026 AT 22:05John McGuirk
February 3, 2026 AT 21:37Heather McCubbin
February 4, 2026 AT 16:07Darren Links
February 6, 2026 AT 08:07