Opioid-Induced Adrenal Insufficiency Risk Calculator
Opioid Risk Assessment
Estimate your risk of opioid-induced adrenal insufficiency (OIAI) based on your treatment duration and dosage.
Risk Assessment
Important: This calculator estimates risk based on clinical guidelines. It does not replace medical diagnosis. If you experience fatigue, dizziness, or low blood pressure while on opioids, consult your healthcare provider immediately.
Opioid-induced adrenal insufficiency (OIAI) is a rare but serious side effect where opioids disrupt the body's stress hormone production. While it affects only a small percentage of users, untreated OIAI can lead to life-threatening complications like Addisonian crisis during stress or surgery. Imagine needing pain relief from opioids but unknowingly risking a hidden hormone problem that could turn deadly during a medical emergency.
What Causes Opioid-Induced Adrenal Insufficiency?
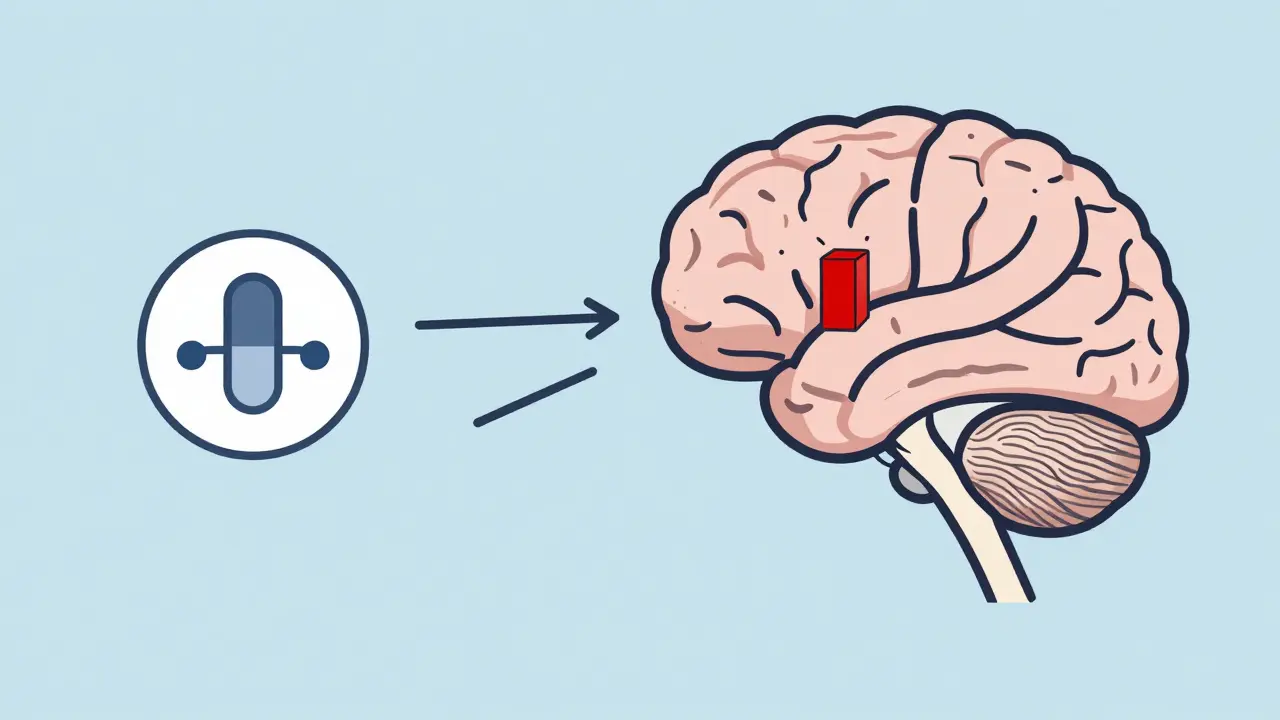
Opioid-induced adrenal insufficiency (OIAI) is caused by opioids blocking the hypothalamic-pituitary-adrenal (HPA) axis. This system controls how your body responds to stress. Normally, when stressed, your brain signals the pituitary gland to release ACTH, which tells your adrenal glands to produce cortisol. But opioids interfere with this communication. Research from Patel et al. (2024) in Frontiers in Endocrinology shows even short-term opioid use can suppress cortisol levels. This isn’t damage to the adrenal glands themselves-it’s the brain’s signaling that’s affected. A 2023 study found about 5% of U.S. adults on chronic opioid therapy had undiagnosed adrenal insufficiency. That’s roughly 1 in 20 people.
Symptoms Often Get Mistaken for Other Issues
Fatigue, nausea, dizziness, low blood pressure, and muscle aches are common in people with chronic pain or opioid withdrawal. But when they stem from OIAI, they can escalate dangerously. For example, a 25-year-old man in Lee et al.’s 2015 case report developed severe hypercalcemia during recovery from a critical illness. Doctors initially thought it was from his pain condition, but tests revealed his cortisol levels were dangerously low due to methadone. Once he stopped methadone and got glucocorticoid replacement treatment, his symptoms resolved. This highlights why confusing OIAI symptoms with other conditions can be deadly.

How Is OIAI Diagnosed?
Diagnosing OIAI requires specific tests. Morning cortisol levels below 3 mcg/dL (100 nmol/L) are a red flag. But recent studies suggest even lower thresholds may be needed. The gold standard is an ACTH stimulation test: injecting synthetic ACTH and measuring cortisol response. A peak cortisol under 18 mcg/dL (500 nmol/L) at 30-60 minutes confirms adrenal insufficiency. However, some clinicians overlook this testing. A 2024 review by Patel noted that many doctors don’t consider OIAI unless patients show extreme symptoms. This is dangerous because early detection prevents emergencies.
Who Is Most at Risk?
High-dose, long-term opioid users. The American Medical Association Ed Hub (2024) states that doses exceeding 20 morphine milligram equivalents (MME) daily significantly increase OIAI risk. A study of 162 chronic opioid users found 5% had OIAI, and those with higher MME doses were more likely affected. De Vries et al. (2020) reported that 22.5% of long-term opioid users failed adrenal stimulation tests compared to 0% of controls. Interestingly, not all opioids carry equal risk. While morphine, oxycodone, and methadone are most commonly linked, fentanyl and tramadol show less evidence of suppression. Still, any opioid used chronically can potentially cause this issue.
Treatment and Reversibility
The good news? OIAI is usually reversible. Stopping or tapering opioids often restores normal hormone production. In severe cases, doctors prescribe glucocorticoid replacement therapy during stressful periods like surgery or illness. Lee et al. (2015) documented a patient whose adrenal function returned to normal within weeks after methadone cessation. However, cortisol has a short half-life (90 minutes), so timing matters. If you’re on opioids and face surgery or infection, tell your doctor about your medication history-they may need to adjust your treatment to prevent crisis.
Why Is OIAI Often Missed?
Clinicians often miss OIAI because symptoms overlap with opioid withdrawal or chronic pain. A 2023 study in the Journal of Clinical Endocrinology & Metabolism found that 60% of OIAI cases were initially misdiagnosed. This is partly due to lack of awareness. Patel et al. (2024) emphasize that "the medical community needs to pay closer attention to opioid-induced hormone suppression" despite established knowledge. Given the opioid epidemic’s scale, even a small percentage of affected patients represents thousands of people at risk.
What is opioid-induced adrenal insufficiency (OIAI)?
Opioid-induced adrenal insufficiency (OIAI) is a condition where long-term opioid use suppresses the body’s ability to produce cortisol, a vital stress hormone. It’s not damage to the adrenal glands themselves but a disruption in the brain’s signaling to those glands. This can lead to dangerously low cortisol levels during physical stress, like surgery or infection.
How common is OIAI among opioid users?
Research shows about 5% of people on long-term opioid therapy have OIAI. However, this varies based on dose and duration. A 2023 study found higher rates in patients taking over 20 morphine milligram equivalents (MME) daily, with up to 22.5% failing adrenal stimulation tests.
What are the symptoms of OIAI?
Symptoms include fatigue, nausea, dizziness, low blood pressure, muscle aches, and unexplained weight loss. These often mimic chronic pain or opioid withdrawal, making diagnosis tricky. In severe cases, untreated OIAI can lead to an Addisonian crisis-characterized by sudden low blood pressure, confusion, and shock.
How is OIAI diagnosed?
Diagnosis requires blood tests: morning cortisol below 3 mcg/dL (100 nmol/L) or a peak cortisol under 18 mcg/dL (500 nmol/L) during an ACTH stimulation test. Many doctors skip these tests because symptoms seem unrelated to hormone issues. If you’re on long-term opioids and experience unusual fatigue or dizziness, ask your doctor about checking cortisol levels.
Can OIAI be reversed?
Yes, in most cases. Stopping or tapering opioids allows the HPA axis to recover. Lee et al. (2015) documented a patient whose cortisol levels returned to normal within weeks after methadone cessation. During recovery, doctors may prescribe temporary glucocorticoid replacement during stressful events like surgery. However, never stop opioids abruptly without medical supervision.
Should I get tested if I’m on opioids?
If you’ve been on opioids for more than 90 days at doses over 20 MME daily, discuss testing with your doctor. Symptoms like unexplained fatigue or dizziness warrant investigation. Early detection prevents life-threatening crises. A 2024 study showed 60% of OIAI cases were missed initially because doctors didn’t consider hormone issues.
What happens if OIAI is left untreated?
Untreated OIAI can lead to an Addisonian crisis during physical stress-like surgery, infection, or injury. This causes sudden low blood pressure, confusion, and organ failure. Without immediate glucocorticoid treatment, it can be fatal. De Vries et al. (2020) confirmed that "untreated adrenal insufficiency can result in severe morbidity and, in case of an untreated Addisonian crisis, even death."
Are certain opioids more likely to cause OIAI?
Morphine, oxycodone, and methadone are most commonly linked to OIAI. Fentanyl and tramadol show less evidence of suppression. However, any opioid used long-term at high doses can potentially cause this issue. A 2023 study found that patients taking over 100 MME daily had triple the risk compared to those on lower doses.
Is OIAI dangerous during surgery?
Absolutely. Surgery is a major physical stressor that triggers cortisol demand. If you have undiagnosed OIAI, your body can’t produce enough cortisol to handle the stress, leading to dangerously low blood pressure or shock. Always inform your surgical team about opioid use. They may need to give you extra glucocorticoids before, during, and after surgery to prevent crisis.

Cole Streeper
February 4, 2026 AT 21:45This is all a government plot to control us. They're using opioids to mess with our adrenal glands so we can't fight back. It's part of the New World Order. They don't want us healthy. Wake up people! This is why we need to stop trusting the system. They're hiding the truth from us. The FDA is in on it. They don't care about your health. They just want to keep you dependent. This is why we need to take back control. It's time to expose this conspiracy. The real danger is the government's agenda. They're trying to make us weak. Don't fall for it! We need to fight this. It's not just about opioids-it's about freedom.
Dina Santorelli
February 5, 2026 AT 11:47This article is just fearmongering. They're trying to scare people into stopping opioids, but it's all made up. I've been on them for years and feel fine. The real problem is the pharma companies pushing fake science. They don't care about real health issues. They just want to make money. This is why people shouldn't trust medical advice anymore. It's all controlled by big pharma. They don't want you to know the truth. This is just another way to control the population. It's all lies. Wake up! The system is broken. They're using this to push their agenda. Don't fall for it. It's all fake.
divya shetty
February 7, 2026 AT 05:25It is imperative that all healthcare providers be educated on this issue. The government must mandate testing for adrenal insufficiency in all patients on opioids. This is a moral obligation to prevent unnecessary deaths. Without proper screening, people will suffer needlessly. We need stricter regulations to ensure patient safety. This is not just a medical issue-it's a human rights issue. Every patient deserves to be informed. The current system is failing. We must act now. This is a call to action for all medical professionals. It's time to prioritize patient health over profit. The stakes are too high to ignore. We cannot let this continue. It's time to hold the system accountable.
Nancy Maneely
February 7, 2026 AT 20:49This is so messed up. Opioids are being used to control our bodies. The government is behind this. I can't believe people don't see it. They want us weak and dependent. This is a travesty. They're hiding the truth. It's all part of the plan. Wake up! They don't care about us. They just want to control us. This is why we need to stop trusting the system. It's time to take back control. Don't fall for it. The real danger is the government's agenda. They're trying to make us weak. It's all lies. This is a conspiracy. We need to fight this.
Phoebe Norman
February 9, 2026 AT 01:54The HPA axis disruption is significant Cortisol suppression is a direct result of opioid use Without proper testing patients are at risk This needs more attention The ACTH stimulation test is critical Many doctors skip it Patients should demand this test It's not just about opioids It's about the body's stress response Cortisol is vital Low levels can be deadly We need better protocols This is a serious issue It's being overlooked We must act This is critical
Albert Lua
February 9, 2026 AT 17:46Glad to see more awareness about this. It's important to talk about these hidden risks. Especially for people on long-term opioids. Sharing knowledge saves lives. This is crucial for patient safety. We need to spread this information. Everyone should know about OIAI. It's not common but it's serious. Doctors need to be aware. Patients should ask questions. Awareness is key. Let's keep talking about it. This is a good step forward. Thanks for sharing!
Katharine Meiler
February 10, 2026 AT 10:26The ACTH stimulation test is critical for diagnosis. Studies show that even low doses can cause suppression. We need standardized protocols for screening. This is a serious issue that's often missed. Patients on opioids should be monitored. Early detection prevents crises. The data is clear. We must prioritize this. It's not just about opioids. It's about adrenal health. This is a medical necessity. Doctors need to be aware. We can't afford to ignore it. This is important for patient safety.
Samantha Beye
February 11, 2026 AT 14:33This is such important information. I've been on opioids for years and never knew about this risk. It's crucial for anyone on long-term therapy to get checked. Doctors need to be more aware. Early detection can prevent life-threatening situations. I'm so glad this is being discussed. It's easy to overlook symptoms like fatigue or dizziness. But they could be signs of something serious. Please talk to your healthcare provider if you have concerns. This knowledge could save your life. Thank you for raising awareness. Let's keep the conversation going. Staying informed is the first step to staying safe.
Rene Krikhaar
February 13, 2026 AT 01:59I've seen cases where this was missed. Always tell your doctor about opioid use before surgery. It can save your life. No joke. The adrenal issue is real. Many doctors don't know about it. They focus on pain management. But this is serious. Cortisol levels drop. You can crash during stress. Get tested if you're on opioids long term. It's not common but it's dangerous. Don't wait until it's too late. Your life depends on it. Talk to your doctor today. This is critical information. Don't ignore it.
Matthew Morales
February 13, 2026 AT 16:05Gotta share this!
Diana Phe
February 14, 2026 AT 23:38This is part of the big pharma agenda. They want to keep us sick. The government is in on it. They don't want us to know the truth about opioids. It's all a conspiracy. They're hiding the facts. Wake up people! This is why we need to fight back. The system is rigged. They control everything. Don't trust the medical establishment. They're lying to you. This is a cover-up. It's time to take action. Don't fall for it. This is a lie. They want us dependent. It's all a scam.
Carl Crista
February 16, 2026 AT 20:09Opioids cause adrenal issues Government knows They don't care Just push more pills It's a control thing End of story They're hiding the truth Wake up This is a conspiracy The system is broken No more trusting them It's time to act They want us weak Don't believe the lies This is real It's dangerous They're lying It's all about control End of story
Jennifer Aronson
February 17, 2026 AT 12:09Interesting article. Important to recognize this rare side effect. Awareness is key. Thanks for the detailed info. This is a serious issue that's often overlooked. Patients on long-term opioids should be tested. Early detection prevents crises. It's crucial for healthcare providers to be informed. This knowledge can save lives. We need more education on this topic. It's not just about opioids. It's about overall health. This is a valuable contribution. Keep sharing important information. Stay informed. Safety first.
Johanna Pan
February 18, 2026 AT 18:29This is really helpful! People need to know about this. I'm glad it's being discussed. Opioids are serious meds. Thanks for the heads up! Awareness can save lives. Always check with your doctor. Better safe than sorry. This is important info. Let's spread the word. Knowledge is power. Stay safe everyone. 😊
lance black
February 19, 2026 AT 16:59Know the risks and get tested to stay safe.