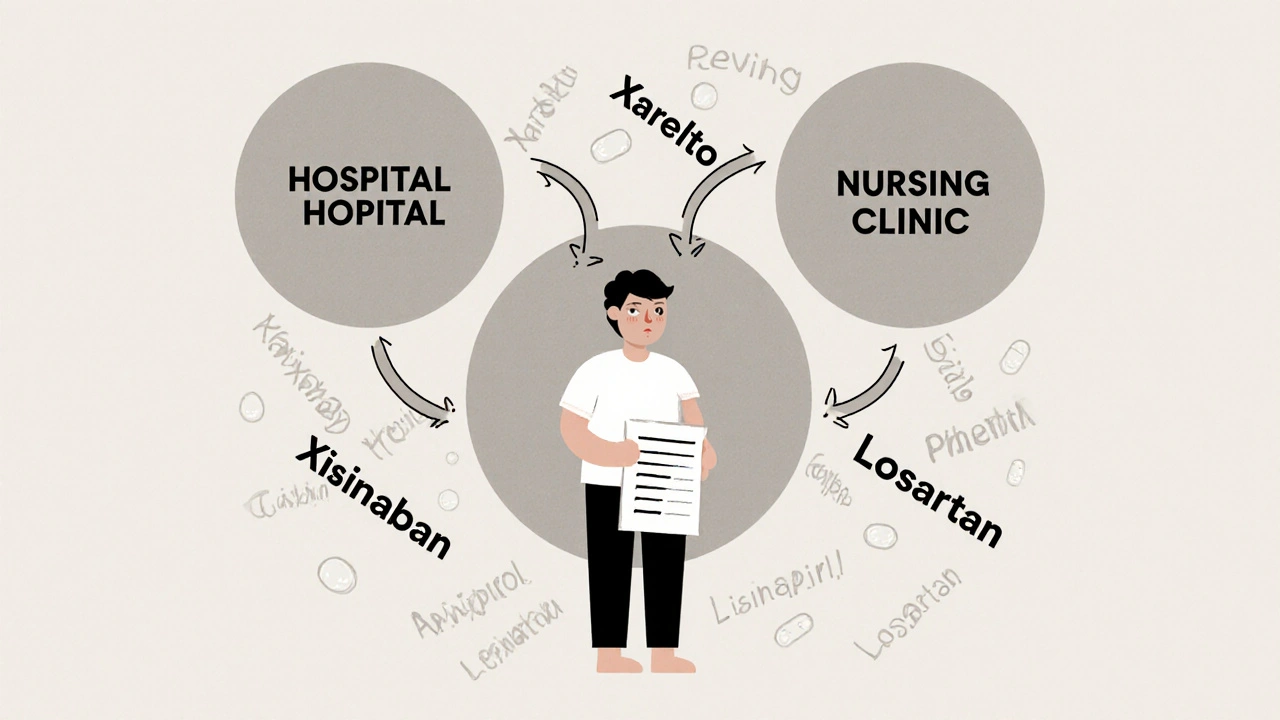
When a patient is prescribed a brand-name blood thinner like Xarelto, but the hospital gives them apixaban instead, it’s not a mistake. It’s a therapeutic substitution-a deliberate switch allowed under institutional formulary policies. These formularies aren’t just lists of approved drugs. They’re living, rule-bound systems that decide which medications get used in hospitals and clinics, why, and when they can be swapped out-even if the doctor didn’t ask for it.
What Exactly Is an Institutional Formulary?
An institutional formulary is a list of medications that a hospital, nursing home, or clinic has officially approved for use. It’s not just a suggestion. It’s a policy with legal weight, especially in places like Florida, where state law (Statute 400.143) requires every long-term care facility to have one. The goal? To make sure patients get safe, effective drugs at the best possible price. These lists are built by a committee: the medical director, the head nurse, and a certified pharmacist. They don’t pick drugs based on what’s cheapest alone. They look at clinical evidence-what actually works, what causes fewer side effects, what’s been proven in real patients. Then they rank them in tiers. Tier 1? Usually generic versions of common drugs, low cost, low patient copay. Tier 3 or 4? More expensive brand names or newer drugs, with higher out-of-pocket costs for the patient. Unlike insurance formularies that decide what your plan will pay for, institutional formularies control what happens inside the facility. If a patient walks in with a prescription for a drug not on the list, the pharmacy can still give it to them-but only if the doctor fills out paperwork explaining why the formulary drug won’t work. That’s called a non-formulary exception.How Therapeutic Substitution Works in Practice
Therapeutic substitution means swapping one drug for another that’s chemically different but expected to do the same job. For example, switching from lisinopril to losartan for high blood pressure. Both are ACE inhibitors or ARBs, both lower blood pressure, but they work slightly differently. The formulary committee decides this swap is safe based on studies showing similar outcomes. In nursing homes, this happens daily. A resident might be on a brand-name statin. The formulary committee, after reviewing cost and safety data, decides to switch them to a generic version. The nurse doesn’t need a new prescription. The pharmacist handles it, as long as the facility’s policy allows it and the patient hasn’t objected. But here’s the catch: this doesn’t always go smoothly. A patient gets switched to a cheaper drug in the nursing home. Then they go to the ER. The ER doctor, unaware of the change, prescribes the original drug. The pharmacy fills it. Now the patient is on two similar drugs at once. That’s when things get dangerous. A 2024 Reddit thread from a hospital pharmacist described a case where a patient was switched from Xarelto to apixaban in a nursing home, then switched back to Xarelto after hospital discharge. No one told the patient. No one updated the primary care doctor. The patient ended up confused, anxious, and at risk for bleeding.Why Facilities Use Formularies: Cost, Safety, and Compliance
The biggest driver? Money. The U.S. spends $600 billion a year on prescription drugs. Institutional formularies help cut that cost without cutting care. According to IQVIA, 89% of all prescriptions in the U.S. are affected by formulary rules. In nursing homes, nearly 94% have formal formularies. But cost isn’t the only reason. Studies show that well-managed formularies reduce adverse drug events by 15-30%. One Florida nursing home director said their quarterly monitoring caught seven dangerous drug interactions in the first year alone-interactions they’d have missed without the system. Florida’s law is strict. Facilities must:- Form a committee within 90 days of starting a formulary
- Write down how they pick drugs and how they monitor outcomes
- Notify prescribers when a substitution happens
- Review data every three months

Where Formularies Work Best-and Where They Struggle
Formularies shine in stable, long-term care settings. Nursing homes, rehab centers, and psychiatric facilities benefit because patients stay for weeks or months. There’s time to monitor effects, adjust, and track outcomes. In acute care hospitals? Not so much. A patient comes in with a heart attack. They need aspirin, clopidogrel, and a statin-now. There’s no time to check the formulary. Doctors don’t want to wait for approval. In these fast-moving environments, formularies are more like guidelines than rules. Many hospitals use them for chronic meds (like diabetes or blood pressure drugs) but leave acute meds open. The bigger problem? Fragmentation. A patient moves from a hospital with one formulary to a nursing home with another. Then back to a primary care clinic with a third. Each system has different rules. Each switch creates confusion. A 2023 AMA survey found that 78% of doctors feel formularies create bureaucratic hurdles when they need to prescribe something outside the list.Who’s Involved-and What They Think
It’s not just pharmacists making these calls. It’s a team:- Pharmacists lead the evaluation, review drug data, and manage substitutions.
- Doctors may support the system for safety but hate the delays when they need a non-formulary drug.
- Nurses are on the front lines. They’re the ones who notice if a patient is confused, dizzy, or having side effects after a switch.
- Patients often don’t know they’ve been switched. AARP says this undermines informed consent. Patients deserve to know when their medication changes-even if it’s “equivalent.”
How Formularies Are Changing-And What’s Next
The rules are evolving. As of January 1, 2025, Florida’s Statute 400.143 expanded monitoring requirements. CMS announced in March 2024 that nursing home formulary compliance will now affect their public quality ratings starting in late 2025. That means hospitals will have even more pressure to get it right. New tools are coming. By 2026, Gartner predicts 80% of healthcare systems will use AI-driven formulary systems that adjust drug choices based on real-time patient outcomes-like if a patient’s blood pressure drops too low after a switch, the system flags it and suggests a change. Some hospitals are even starting to use genetic data. If a patient has a gene variant that makes them metabolize a drug slowly, the formulary might automatically avoid that drug. Deloitte found that 72% of healthcare executives plan to use pharmacogenomics in formulary decisions within five years. But the biggest challenge? Lack of standardization. Right now, 32 states have their own rules for institutional formularies. Florida’s are the strictest. Others are looser. That creates chaos when patients move across state lines.What Patients and Families Should Know
If you or a loved one is in a hospital or nursing home:- Ask: “Is this the drug my doctor prescribed, or was it switched?”
- Ask: “Why was it changed?”
- Ask: “Can I get the original drug if I prefer it?”
- Keep a personal medication list and update it after every switch.
- Share your list with every new provider-even if they’re in a different building.
Implementation Challenges and How Facilities Are Solving Them
Getting a formulary system up and running isn’t easy. Sixty-eight percent of facilities report problems integrating it with their electronic health records (EHR). The system might not alert staff when a substitution happens. Or it might flag too many alerts, so people start ignoring them. Solutions? Work with your EHR vendor to build smart alerts. For example, if a patient is switched from one blood thinner to another, the system should pop up a note for the nurse: “Therapeutic substitution: Xarelto → Apixaban. Monitor for bleeding.” Training is also critical. Nursing staff need at least four to eight weeks to learn the new workflow. Pharmacists need certification under Florida Statute 465.0125. Medical directors need experience in formulary governance. And documentation? It’s not optional. Facilities must update their policies at least once a year. On average, they spend 20-30 hours per quarter just maintaining the system. Resources like the AMCP Formulary Management Toolkit and Florida’s Formulary Implementation Guide are used by 85% of hospital pharmacy directors. They’re not nice-to-haves-they’re essential.Are institutional formularies legal?
Yes. Institutional formularies are legally required in states like Florida under Statute 400.143. They’re also widely used across the U.S. under federal guidelines. As long as they’re managed by a qualified committee, follow evidence-based standards, and allow for exceptions when medically necessary, they’re fully compliant.
Can a patient refuse a therapeutic substitution?
Yes. Patients have the right to refuse any medication change, even if it’s on the formulary. If a patient or their legal representative objects, the facility must honor that request and provide the originally prescribed drug-even if it’s more expensive. Documentation of the refusal is required.
Do formularies save money without hurting care?
Studies show they can. By favoring generic drugs and eliminating ineffective or overly expensive options, formularies reduce costs by up to 30% in some settings. At the same time, they lower adverse drug events by 15-30% because they remove drugs with poor safety records. The key is using evidence, not just price, to make decisions.
Why do some doctors hate formularies?
Because they can delay care. Getting a non-formulary drug approved often requires paperwork, phone calls, and waiting days. For patients with complex conditions-like rare autoimmune diseases or treatment-resistant depression-those delays can be dangerous. Many doctors feel formularies prioritize cost over clinical judgment.
How often are formularies updated?
At least once a year, but many facilities update them quarterly or even monthly. The American Society of Health-System Pharmacists now recommends bi-monthly reviews. Updates happen when new drugs are approved, when safety warnings are issued, or when cost savings become significant.
Do all hospitals use formularies?
No. While 94% of nursing homes use formal formularies, only about 78% of acute care hospitals do. Smaller clinics and rural hospitals may rely on simpler lists or follow their insurance plan’s formulary instead. But the trend is moving toward formal systems, especially as value-based care becomes more common.




Rachael Gallagher
November 24, 2025 AT 10:40This is just another way the system screws patients while pretending to save money. They swap your meds like trading cards and then act like you should be grateful. I’ve seen people get confused, dizzy, even bleed because some pharmacist decided they knew better than the doctor. This isn’t healthcare-it’s corporate rationing with a lab coat.
steven patiño palacio
November 25, 2025 AT 09:07Formularies are necessary, but they need transparency and patient-centered safeguards. The fact that patients aren’t informed of substitutions is unacceptable. Pharmacists and clinicians should be required to document and communicate changes in plain language. It’s not just about cost-it’s about trust and autonomy. We can optimize care without eroding patient rights.
stephanie Hill
November 27, 2025 AT 02:20Ever wonder why your meds change every time you switch facilities? It’s not just about cost-it’s the pharmaceutical industry pulling strings behind the scenes. Big Pharma pays formulary committees to push certain drugs. Then they jack up prices on the ones they *don’t* want you on. The FDA? They’re asleep at the wheel. Your doctor doesn’t even know what’s happening. This is how they control you. Wake up.
Akash Chopda
November 29, 2025 AT 01:46Alex Dubrovin
November 30, 2025 AT 08:20Natashia Luu
November 30, 2025 AT 14:09It is deeply concerning that institutional formularies, while ostensibly designed for cost containment and clinical efficacy, frequently operate without adequate patient notification or informed consent. This constitutes a fundamental breach of medical ethics and violates the principle of patient autonomy. Such practices, if left unregulated, represent a systemic erosion of the physician-patient relationship.
akhilesh jha
November 30, 2025 AT 22:22I work in a rural clinic. We don’t even have a full-time pharmacist. Our "formulary" is a printed sheet from 2019 taped to the fridge. We give what’s in stock. Patients get switched because the pharmacy ran out, not because of a committee decision. The whole system breaks down outside big hospitals. And nobody’s talking about that.
Jeff Hicken
November 30, 2025 AT 23:31