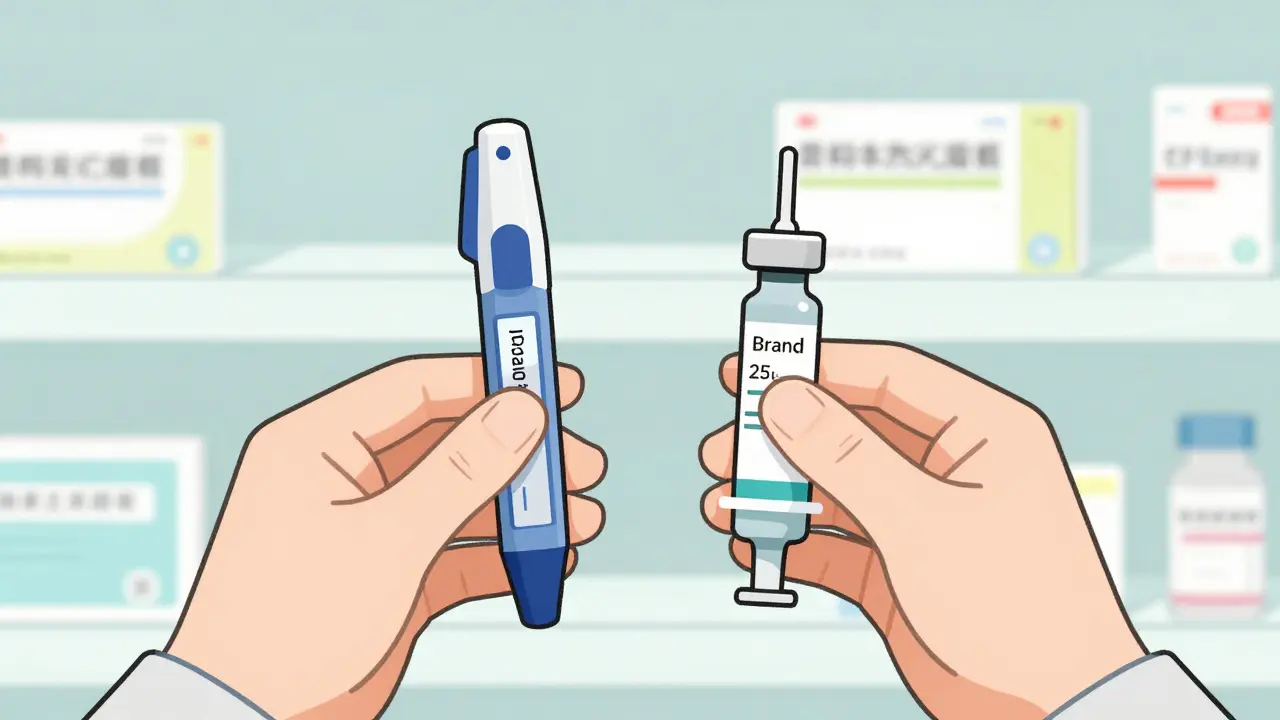
Imagine you need an EpiPen. Your doctor prescribes it. You go to the pharmacy and get a generic version - but it doesn’t work the same way. The epinephrine is cheaper, yes. But the auto-injector? Still the brand name. Or worse - the generic injector doesn’t even exist yet. You pay almost as much as if you’d bought the brand. Why? Because generic combination products aren’t like regular generics. When a drug and a device are built to work together, swapping one part doesn’t mean you’ve swapped the whole thing.
What Exactly Is a Combination Product?
A combination product isn’t just two things in the same box. It’s a drug, a device, or a biological product fused together - physically, chemically, or by design - to serve one medical purpose. Think of insulin pens, inhalers with built-in dose counters, auto-injectors like EpiPens, or prefilled syringes. These aren’t just drugs with packaging. The device is part of the treatment. If the device fails, the drug doesn’t work - even if it’s perfectly made.The U.S. Food and Drug Administration (FDA) has a special office for these: the Office of Combination Products. Created in 2002, it decides whether a product is mainly a drug, a device, or a biologic - and which center reviews it. That’s important. If the main action comes from the drug, it goes to CDER (Center for Drug Evaluation and Research). If the device does the heavy lifting - like a pacemaker delivering a drug - it goes to CDRH (Center for Devices and Radiological Health). This decision shapes everything: how long approval takes, what data you need, and whether a generic version can even be approved.
Why Can’t You Just Swap the Drug?
Regular generic drugs are easy. You copy the active ingredient. Prove it’s the same. Done. But with combination products, the game changes. The FDA requires more than chemical equivalence. You have to prove the entire system works the same way.Take the EpiPen. The generic version isn’t just epinephrine in a vial. It’s epinephrine in a specific auto-injector that delivers the right dose at the right speed, with the right force, and the right safety features. If the needle length, spring tension, or trigger mechanism is even slightly off - the dose might be too low, too late, or too dangerous. That’s why the FDA demands a full human factors engineering study. You don’t just test the device in a lab. You test it with real people - including those with arthritis, shaky hands, or panic attacks - to make sure they can use it correctly every time.
And here’s the catch: even if you have a generic drug and a generic device, they might not be approved to work together. Each component might be approved separately, but only one company has the rights to combine them. That means you can’t legally substitute a generic drug with a branded device - even if the patient has both. The system isn’t designed for piecemeal swaps. The FDA calls this “therapeutic equivalence,” and for combination products, it’s much harder to prove.
The Data Doesn’t Lie: Fewer Generics, Higher Prices
In 2023, over 90% of all prescription drugs in the U.S. were generics. But for combination products? Only 12% are generic. That’s not a typo. Branded versions still control 68% of the market. Why? Because development is brutal.Creating a generic version of a drug-device combo takes 18 to 24 months longer than a regular generic. Costs jump by $2.1 million to $3.7 million. And even then, nearly half of all applications get rejected - mostly because the device comparison data is incomplete. Between 2020 and 2023, 43% of rejected applications cited poor device analysis. That’s not a small oversight. It’s a systemic flaw.
And it’s not just manufacturers who suffer. Patients pay the price. On average, patients pay 37% more out-of-pocket for complex combination generics than for regular generics. Pharmacists report that 68% have seen patients confused or denied substitutions. One Reddit user summed it up: “Why can’t my generic EpiPen substitute normally?” The answer? Because the device isn’t generic yet - and even if it is, it might not be approved to work with that specific drug.
Who’s Affected the Most?
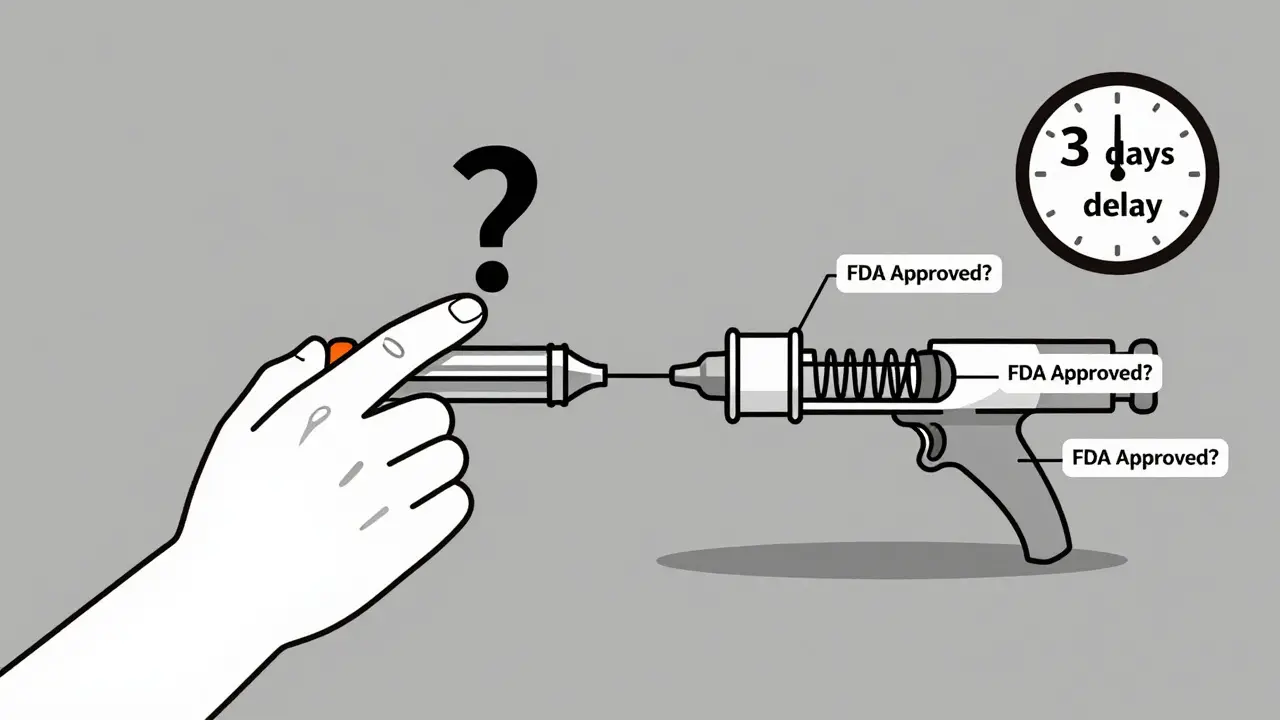
It’s not just people with allergies. Think diabetics using insulin pens. Asthma patients with inhalers. Heart patients with drug-eluting stents. Cancer patients on prefilled chemotherapy syringes. These aren’t niche cases. They’re millions of people relying on devices that are as critical as the drugs themselves.Healthcare providers are caught in the middle. A 2024 AMA survey found that 57% of doctors have seen treatment delays because pharmacists couldn’t substitute a combination product. The average delay? Over three business days. That’s three days without treatment. For someone with anaphylaxis risk or unstable diabetes, that’s dangerous.
And the problem is growing. Patient advocacy groups documented 217 cases in 2023 where people couldn’t access a therapeutic equivalent - up 29% from the year before. The trend is clear: as more drugs get combined with devices, the substitution system is falling further behind.
What’s Changing? Slowly.
The FDA knows this is broken. In April 2024, they released new guidance on how to submit comparative device analyses. In June 2024, Commissioner Robert Califf launched “Complex Generic Initiative 2.0” - a push to cut approval times by 30% by 2026. They’ve added 32 new reviewers just for combination products.States are stepping in too. California and Massachusetts passed laws requiring pharmacists to be able to substitute combination products if they’re deemed therapeutically equivalent. Other states are following. The Generic Pharmaceutical Association says 14 states are now working on similar bills.
But progress is slow. Only 17 companies have successfully brought generic combination products to market - compared to over 120 for regular generics. The market is dominated by a handful of players because the cost and risk are too high for smaller firms.
What Does This Mean for You?
If you’re a patient: don’t assume your generic prescription will work the same as the brand. Ask your pharmacist: “Is this the full generic combination? Or just the drug?” If the device is still branded, ask if there’s a fully generic alternative - and if not, why not.If you’re a prescriber: write prescriptions clearly. Don’t just say “epinephrine auto-injector.” Specify the brand or the generic product name. That way, the pharmacist knows exactly what to dispense - and can flag substitution issues before they become emergencies.
If you’re a caregiver or advocate: push for transparency. Demand that manufacturers and regulators make it clear which parts of a combination product are generic - and which aren’t. Patients deserve to know what they’re getting - and why it might cost more.
The Bottom Line
Generic combination products aren’t just another type of generic. They’re a new category of medicine - one that blends chemistry, engineering, and human behavior. The old rules don’t apply. You can’t just swap a pill. You have to swap the whole system.Until the laws, the systems, and the market catch up, patients will keep paying more, waiting longer, and risking gaps in care. The promise of generics - lower cost, wider access - is still out of reach for millions. The solution isn’t just more regulation. It’s smarter regulation. One that treats the device and the drug as one unit - not two separate parts.
Can I substitute a generic drug with a branded device in a combination product?
No. Even if the drug is generic and the device is branded, the FDA does not consider this a substitution. Combination products are approved as complete systems. Mixing components from different manufacturers - even if both are approved - is not legally or therapeutically equivalent. Pharmacists are required to dispense the exact product prescribed unless a fully approved generic combination product exists.
Why are generic combination products so expensive?
Because they’re incredibly hard to develop. Unlike regular generics, you must prove the entire device-drug system works identically to the brand. This requires human factors testing, comparative device analysis, and years of development. Costs average $2.1-3.7 million and take 18-24 months longer than standard generics. Few companies can afford it, so competition stays low - and prices stay high.
How do I know if my generic prescription is a full combination product?
Check the product name on the packaging. If it matches the brand name exactly (e.g., “Adrenaclick” instead of just “epinephrine”), it’s likely the full generic combination. If it only lists the drug name (e.g., “epinephrine injection”), the device may still be branded. Ask your pharmacist to confirm whether both the drug and device components are generic and FDA-approved as a matched pair.
Are there any combination products that have good generic competition?
Yes - but they’re rare. Inhalers for asthma and COPD have seen better generic adoption, with about 38% market penetration. This is because the device design is simpler and easier to replicate. Auto-injectors and prefilled syringes lag far behind, with only 19% generic use. The complexity of the device determines how quickly generics can enter the market.
What’s being done to fix this problem?
The FDA launched the Complex Generic Initiative 2.0 to speed up approvals and added 32 new reviewers. Fourteen states are updating laws to allow substitution of therapeutically equivalent combination products. Industry groups are pushing for clearer guidance. But progress is slow. Real change will require manufacturers to invest in these products - and regulators to treat the device and drug as one unit, not two separate entities.
What Comes Next?
The future of combination products depends on three things: better regulation, more investment, and clearer communication. Until patients, pharmacists, and doctors understand that a combination product isn’t just a drug - it’s a system - the gap between promise and reality will stay wide.More approvals are coming. More states will pass substitution laws. More companies will try to enter the market. But until the FDA and Congress treat these products as what they are - integrated medical systems - patients will keep paying more, waiting longer, and risking gaps in care.
The goal isn’t just to make generics cheaper. It’s to make them work - fully, safely, and without confusion.


Julie Chavassieux
December 22, 2025 AT 07:56This is why I stopped trusting generics entirely. I got a "generic" EpiPen last year and it jammed. I swear, the device felt like it was made by someone who’d never held a human hand before. Now I pay full price. No more gambling with my life.
Jeremy Hendriks
December 22, 2025 AT 11:16Let’s be real - this isn’t about innovation or safety. It’s about patent trolling disguised as regulation. The FDA lets brand-name companies lock down device designs like proprietary software. Meanwhile, real patients bleed money while CEOs sip champagne. The system isn’t broken - it’s designed this way. And the worst part? We’re all complicit because we’re too tired to fight it.
Nader Bsyouni
December 24, 2025 AT 05:37So you’re telling me the entire healthcare system is just a corporate theater where the only real actors are lawyers and shareholders? And we’re the audience paying for front-row seats? Fascinating. The tragedy isn’t the lack of generics - it’s that we still believe in the myth of competition
jenny guachamboza
December 25, 2025 AT 10:57OMG I KNEW IT 😱 The FDA is in on it!!! I read on a blog that Big Pharma pays off regulators to keep device patents alive forever!!! They even use microchips in the injectors to track you!!! 🤯 #FreeTheEpiPen #ConspiracyIsReal
Tarun Sharma
December 26, 2025 AT 05:31This is a well-documented issue. The regulatory framework for combination products requires significant technical and clinical validation. It is not a matter of corporate greed but of scientific rigor. Premature substitution may pose risks to patient safety.
Kiranjit Kaur
December 27, 2025 AT 13:18I’m so glad someone finally put this into words 💙 My mom’s insulin pen broke last winter and the pharmacy couldn’t swap it - she had to wait 5 days. That’s 5 days of stress, panic, and missed doses. We need change - not just for her, but for everyone. Let’s push for better laws and clearer labels. We can do this 🙌
Jim Brown
December 28, 2025 AT 07:35One cannot help but observe that the confluence of pharmaceutical science and biomedical engineering has outpaced the legislative and regulatory apparatus designed to govern it. The reductionist paradigm of treating the drug and device as discrete entities is epistemologically flawed - and ethically indefensible. The combination product is an emergent system; its therapeutic efficacy is not merely additive, but integrative. To permit substitution of partial components is to engage in therapeutic nihilism disguised as cost-efficiency.
Sam Black
December 28, 2025 AT 17:34As someone who’s helped design inhaler prototypes, I can tell you - the device isn’t just packaging. It’s the delivery mechanism for trust. If the patient can’t use it reliably under stress, the drug is useless. That’s why human testing matters. But we need simpler pathways for generics. Small companies can’t afford $3M studies. Maybe open-source device specs? Let’s build a commons.
Cara Hritz
December 29, 2025 AT 19:05Wait so if the device is branded but the drug is generic then it’s NOT a generic? But my bottle says "epinephrine" so I thought it was?? I’ve been getting ripped off?? 😭
Jamison Kissh
December 31, 2025 AT 04:25What if we treated combination products like smartphones? You don’t swap the battery from one brand into another and expect it to work the same. The software, the hardware, the user interface - they’re all tuned together. Why should medicine be any different? The real problem isn’t regulation. It’s our assumption that everything should be modular. Maybe some things are meant to be whole.