Medical Term Translator
Understand Your Medical Records
Enter medical terms or codes from your health records to see plain language explanations. This tool helps bridge the gap between clinical jargon and patient understanding.
Why Your Doctor’s Notes Don’t Sound Like You
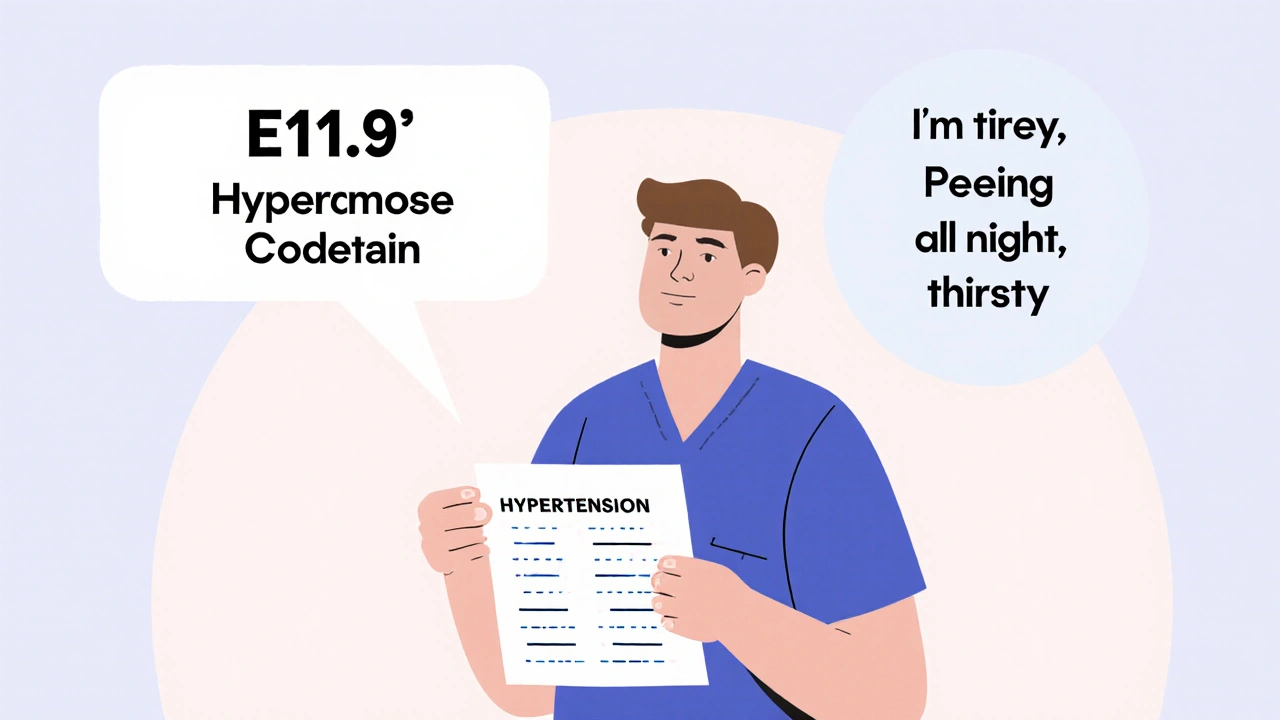
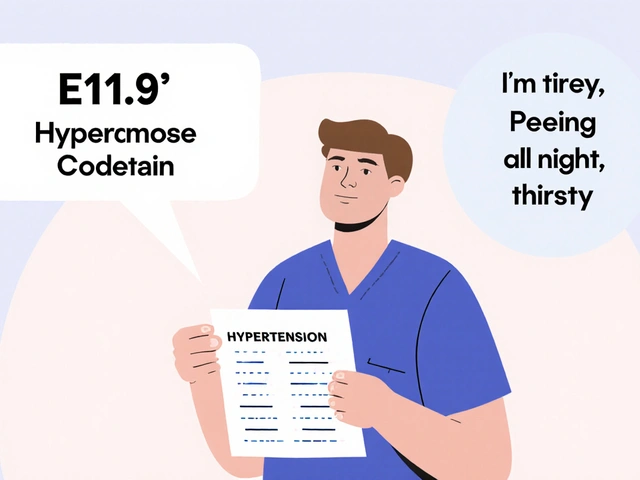
You get your lab results back. Your doctor wrote "Type 2 Diabetes Mellitus, E11.9". You read it and feel confused. Was that a diagnosis? A warning? A judgment? You didn’t say "E11.9". You said, "I’m always tired, I’m peeing all night, and I can’t stop drinking water."
This isn’t just a mismatch in words. It’s a gap in understanding that’s been hiding in plain sight for decades. Healthcare providers use coded language to document care. Patients use lived experience to describe illness. And when those two worlds collide - in charts, portals, and conversations - misunderstandings happen. Often, they lead to missed meds, avoided appointments, and even harm.
How Providers Label: Codes, Charts, and Compliance
When a doctor writes in an Electronic Health Record (EHR), they’re not just telling a story. They’re coding for billing, research, and legal protection. That’s why you see terms like ICD-10 and CPT codes. ICD-10 has over 70,000 diagnosis codes. CPT has more than 10,000 procedure codes. These aren’t random. They’re standardized. Every code maps to a specific payment rate, insurance rule, or public health statistic.
Systems like Epic and Cerner - used by more than half of U.S. hospitals - are built around these codes. They help hospitals get paid. They help researchers track disease trends. But they don’t help you understand why you feel awful.
Providers are trained to use precise language. "Hypertension" instead of "high blood pressure." "Dyspnea" instead of "I can’t catch my breath." It’s efficient. It’s accurate. But it’s not human.
How Patients Experience: Stories, Symptoms, and Fear
Patients don’t think in codes. They think in sensations and fears. "My chest feels tight when I walk up the stairs." "I’ve been dizzy for three weeks and no one listens." "I’m scared this pill will make me sick again."
A 2019 study in the Journal of General Internal Medicine found that 68% of patients didn’t understand common medical terms. Forty-two percent didn’t know "hypertension" meant high blood pressure. Sixty-one percent couldn’t define "colitis." That’s not ignorance. That’s poor communication.
And when patients see terms like "poorly controlled DM" in their portal, they don’t think "diabetes management needs adjustment." They think, "I’m failing. I’m not doing enough." One patient on PatientsLikeMe wrote, "I thought my chart said I was a bad person, not that my sugar was high."
That’s the emotional cost of mislabeled information. It doesn’t just confuse - it shames.
The Bridge: Health Information Management Professionals
There’s a hidden group of people working behind the scenes to fix this. They’re called Health Information Management (HIM) professionals. These are the coders, transcriptionists, and data stewards who translate provider notes into structured data - and sometimes, back into plain language.
They’re certified by AHIMA and trained in both medical terminology and patient privacy laws like HIPAA and the HITECH Act. Their job? Make sure records are complete, accurate, and protected. But increasingly, they’re also asked to make them understandable.
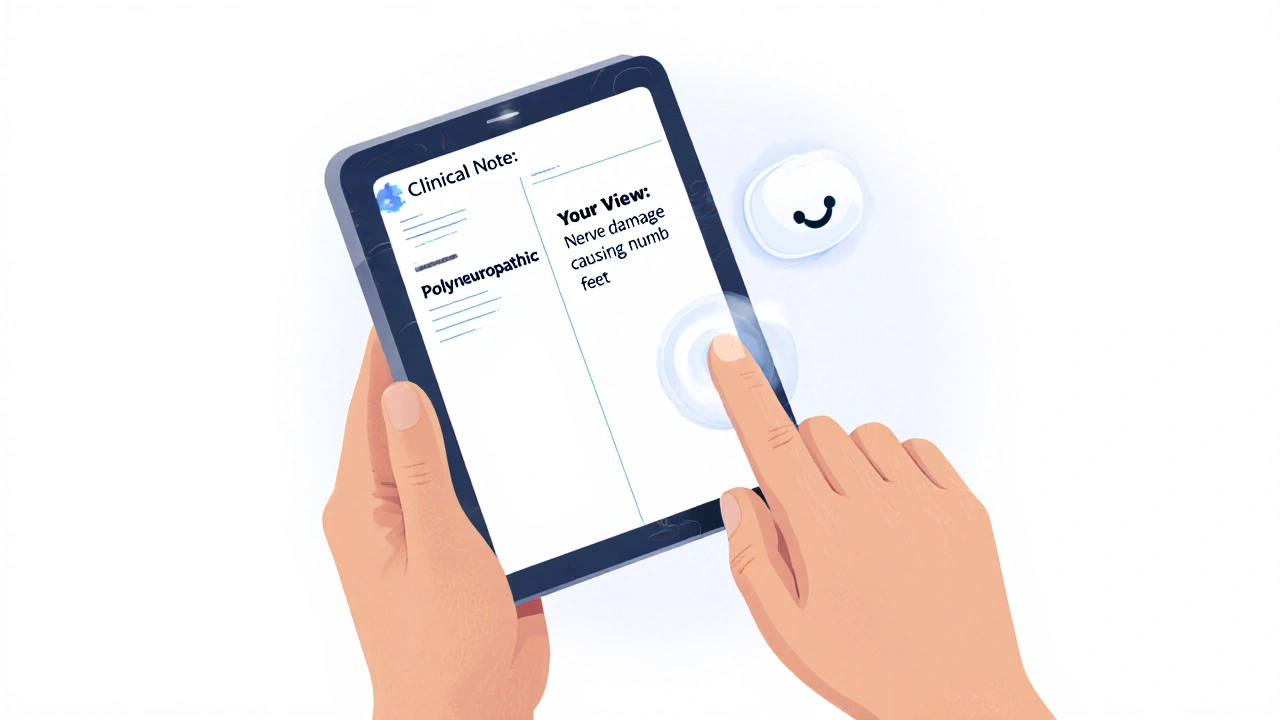
They’re the ones who ensure 95% coding accuracy for Medicare reimbursement. They’re also the ones who help hospitals design patient-friendly versions of clinical notes - translating "myocardial infarction" to "heart attack," or "polyneuropathy" to "nerve damage causing numbness in feet."
Real-World Consequences: When Labels Cause Harm
The numbers don’t lie:
- 30-40% of medication errors come from communication breakdowns, according to Dr. Thomas Bodenheimer.
- 57% of patients feel confused by medical terms in their records (American Medical Association, 2022).
- 32% avoid follow-up care because they don’t understand what’s written.
- 64% of doctors spend 15-30 minutes per visit just explaining terms.
It’s not just about confusion. It’s about trust. When patients don’t understand their records, they stop trusting them. And when they stop trusting their records, they stop trusting their care.
One hospital system found that after patients could read their own notes - through the OpenNotes initiative - medication adherence went up 19%. Confusion about diagnoses dropped 27%. That’s not magic. That’s clarity.
What’s Changing: New Rules, New Tools
Things are shifting - fast.
The 21st Century Cures Act (2016) forced providers to give patients access to their clinical notes without editing. By April 2021, that became law. Suddenly, patients could see everything - including terms they didn’t understand.
So hospitals had to adapt. Today, 89% of U.S. hospitals let patients view their notes - up from just 15% in 2010. And now, more than 55 million patients across 350+ organizations can see their records through OpenNotes.
New standards are helping too. The WHO’s ICD-11, launched in 2022, now includes patient-friendly descriptions alongside clinical codes. The HL7 FHIR standard - adopted by 78% of major U.S. health systems - lets EHRs show two versions of the same note: one for providers, one for patients.
And now, AI is stepping in. Google’s Med-PaLM 2 can convert clinical notes into plain language with 72.3% accuracy. It’s not perfect yet - 95% is the goal for clinical use - but it’s a start.
What Works: Plain Language, Teach-Back, and Trust
There’s no single fix. But there are proven strategies:
- Plain language templates - Mayo Clinic’s pilot program reduced patient confusion by 38% by auto-translating medical terms in patient-facing documents.
- Teach-back method - providers ask patients to repeat back what they heard. A 2018 JAMA study showed it cuts miscommunication by 45%.
- OpenNotes - when patients see notes in real time, they ask better questions, take meds as prescribed, and feel more in control.
It’s not about dumbing down medicine. It’s about speaking clearly. You wouldn’t hand someone a manual written in Mandarin and expect them to fix their car. Why do we expect patients to understand medical jargon without translation?
The Future: When Systems Speak Both Languages
By 2027, the American Medical Informatics Association predicts 60% of EHRs will have real-time terminology translation built in. Imagine logging into your portal and seeing:
Provider note: "E11.9 - Type 2 Diabetes Mellitus, without complications" That’s the goal. Not to erase medical language - but to add a second layer. One that speaks to the person, not just the diagnosis. This isn’t a tech problem. It’s a human one. And fixing it means recognizing that your story matters as much as your code. Doctors use medical terms because they’re precise, standardized, and required for billing, legal records, and research. Systems like ICD-10 and CPT codes ensure consistency across hospitals and insurance claims. But that doesn’t mean they’re meant for patients. The problem isn’t the jargon itself - it’s when patients never get a plain-language version. Yes - and you should. Many hospitals now offer patient-friendly versions of notes automatically. If yours doesn’t, ask your provider or the medical records department. You have the right to understand your health information. Saying "I don’t understand this term" isn’t being difficult - it’s being responsible for your care. ICD-10 codes describe diagnoses - like "Type 2 Diabetes" or "High Blood Pressure." CPT codes describe procedures - like "blood test," "MRI," or "annual physical." ICD-10 tells what’s wrong. CPT tells what was done. Both are used for billing, but only ICD-10 is used to track disease patterns in public health. OpenNotes lets patients read their doctors’ visit notes in real time - before, during, or after the appointment. Studies show that when patients see what’s written, they remember instructions better, take meds correctly, and feel more involved in decisions. Some hospitals now add side-by-side translations: clinical terms on one side, plain language on the other. AI tools like Google’s Med-PaLM 2 can convert clinical notes into plain language with good accuracy - around 72%. But they’re not ready to replace human judgment. The goal isn’t to automate understanding - it’s to support it. AI can suggest translations, flag confusing terms, and help HIM staff work faster. But only a human can know if a translation feels right to a patient. Don’t pretend you get it. Write down the terms you don’t understand. Call your provider’s office and ask for a plain-language explanation. Many clinics have patient navigators or health educators who specialize in this. You can also ask for a copy of your records and bring them to a trusted friend or family member to help you read them. Understanding your health isn’t optional - it’s your right.
Patient view: "You have type 2 diabetes. Your body doesn’t use insulin well. We’ll help you manage it with diet, movement, and medicine."
Why do doctors use medical jargon instead of plain language?
Can I ask my doctor to rewrite my medical notes in plain language?
What’s the difference between ICD-10 and CPT codes?
How does OpenNotes help patients understand their records?
Is AI going to fix the labeling gap between patients and providers?
What should I do if I don’t understand my medical records?

Meghan Rose
November 6, 2025 AT 07:27Steve Phillips
November 7, 2025 AT 15:57Rachel Puno
November 9, 2025 AT 14:37Clyde Verdin Jr
November 10, 2025 AT 07:00Key Davis
November 10, 2025 AT 22:35Cris Ceceris
November 11, 2025 AT 20:28Brad Seymour
November 13, 2025 AT 04:00Erika Puhan
November 13, 2025 AT 16:24Edward Weaver
November 13, 2025 AT 23:47Lexi Brinkley
November 15, 2025 AT 13:32Kelsey Veg
November 16, 2025 AT 19:44Alex Harrison
November 17, 2025 AT 03:29Jay Wallace
November 17, 2025 AT 14:06Alyssa Fisher
November 18, 2025 AT 16:30