What Is a Kidney Transplant?
A kidney transplant is when a healthy kidney from a donor replaces a failing one. It’s not just a last resort-it’s often the best option for people with end-stage renal disease (ESRD). Unlike dialysis, which keeps you alive but doesn’t restore normal function, a transplant lets you live more freely, with better energy, fewer dietary limits, and a much higher chance of surviving long-term.
By 2023, over 27,000 kidney transplants were done in the U.S. alone. The success rate? Around 95% of transplanted kidneys are still working one year later. For those who get a kidney from a living donor, that number climbs to 97%. Five years out, about 85% of living donor kidneys are still functioning. That’s far better than the 50% survival rate for people staying on dialysis long-term.
Who Qualifies for a Kidney Transplant?
You don’t need to be perfect to qualify-but you do need to be well enough to survive surgery and stick with lifelong care. Most centers require you to have ESRD, meaning your kidneys are working at 15% or less of normal capacity. That’s measured by your glomerular filtration rate (GFR), which should be 20 mL/min or lower. Some centers, like Mayo Clinic, will consider you even if your GFR is up to 25 mL/min if your kidney function is dropping fast or you have a living donor ready.
Age isn’t a hard barrier. While Vanderbilt University won’t routinely list patients over 75, UCLA and others evaluate older adults individually. What matters more is your overall health. If you’re active, mentally sharp, and have support at home, you could be a strong candidate-even in your 80s.
What Disqualifies Someone?
Not everyone who needs a transplant can get one. Certain conditions make the risk too high. Active cancer is an absolute no-go unless you’ve been cancer-free for a set period (usually 2-5 years, depending on the type). Untreated infections like tuberculosis or hepatitis B with active virus in your blood also block eligibility. HIV isn’t automatically a barrier anymore-if your viral load is undetectable and your CD4 count is above 200, you can still be considered.
Obesity is a major factor. A BMI over 45 is an outright disqualification at most centers. At Vanderbilt, a BMI above 35 is a red flag. Why? Fat increases surgical risks by 35% and raises the chance of the new kidney failing by 20%. Many centers require weight loss before surgery.
Heart and lung health matter too. If your right heart pressure (RVSP) is over 50 mm Hg, or your lung pressure (PAS) hits 70 mm Hg or higher, you’re typically ruled out. Needing oxygen all the time because of COPD? That’s also a dealbreaker. Your heart must pump well enough-ejection fraction above 35-40% is usually required.
The Evaluation Process
Getting approved isn’t just about blood tests. It’s a full picture of your life. You’ll go through:
- Blood tests for infections, tissue type, and kidney function
- Cancer screenings like colonoscopies and skin checks
- Heart tests: echocardiograms, stress tests, sometimes a cardiac catheter
- Psychological evaluation to make sure you can handle the stress and responsibility
- Financial and social review-do you have someone to help you take pills, get to appointments, and notice if something’s wrong?
Frailty is now a key part of the check. Centers like Vanderbilt use the Fried Frailty Criteria: unintentional weight loss, constant tiredness, weak grip, slow walking, low activity. If you score high on this, they may delay or deny the transplant-not because you’re too old, but because your body might not recover.
And yes, you need a care partner. Nebraska Medicine and others require someone who’ll be your backup-reminding you to take meds, driving you to follow-ups, calling the clinic if you feel off. No one survives a transplant alone.

What Happens During Surgery?
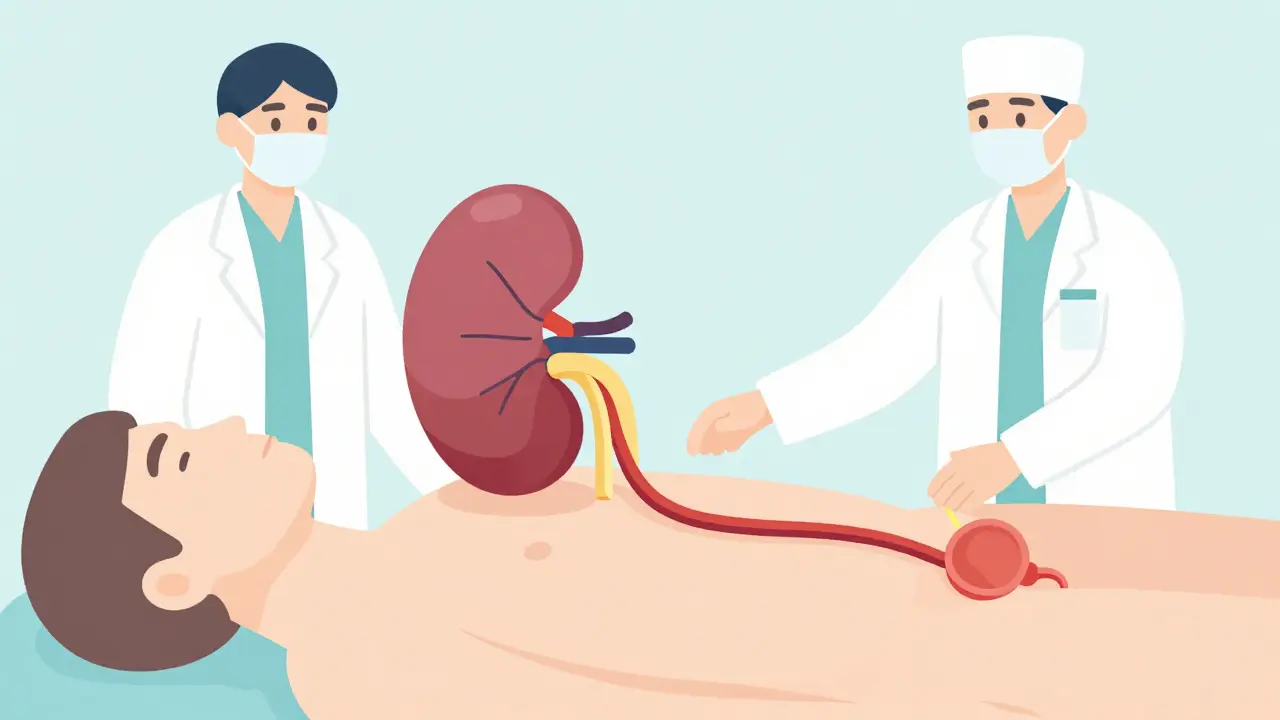
The surgery takes 3 to 4 hours. You’re under full anesthesia. The new kidney goes into your lower belly-not where your old kidneys are. The surgeon connects its blood vessels to your pelvic arteries and veins, then attaches the ureter (the tube that carries urine) to your bladder. Your own kidneys? Usually left in place unless they’re infected, bleeding, or causing pain.
Most transplanted kidneys start working right away. But in about 20% of cases-especially with kidneys from deceased donors-the new organ takes a few days to start producing urine. That’s called delayed graft function. You might need dialysis for a week or two until it kicks in. It’s not failure. It’s just a slow start.
Life After Transplant: The Lifelong Commitment
Getting a new kidney isn’t the end. It’s the beginning of a new routine. You’ll take immunosuppressants every single day, for the rest of your life. These drugs stop your immune system from attacking the new organ. The standard combo? A calcineurin inhibitor (like tacrolimus), an antiproliferative drug (like mycophenolate), and a steroid (like prednisone). Some people get extra antibodies at the start to reduce early rejection risk.
These drugs have side effects. You might gain weight, get high blood pressure, have shaky hands, or face higher risks of infection or skin cancer. But the trade-off? You’re alive and off dialysis.
Follow-up is strict. Weekly visits for the first month. Then monthly for the next few months. After six months, you’ll typically see your team every three months. Once you’re stable, you’ll still need annual blood work, ultrasounds, and check-ins.
Don’t skip your appointments. Rejection can happen without symptoms. By the time you feel sick, it might be too late. Blood tests catch it early. A simple rise in creatinine can signal trouble before you even notice.
Living vs. Deceased Donor: The Big Difference
Not all transplants are the same. A kidney from a living donor lasts longer and works better. Why? It’s healthier, transplanted immediately, and doesn’t sit in cold storage for hours. The 1-year survival rate? 97% for living donor kidneys. For deceased donor kidneys? 93%. Five-year survival? 85% vs. 78%.
Living donors can be family, friends, or even strangers. They don’t need to be a perfect match anymore. Modern drugs make cross-matching less critical. And the donor’s risk? Very low. Most live normal, healthy lives afterward.
Waiting for a deceased donor? The average wait in the U.S. is 3-5 years. In the UK, it’s similar. That’s why living donation is so powerful. If you have someone willing, you can skip the wait-and get a better outcome.
What’s New in Kidney Transplants?
Technology is improving. The Kidney Donor Profile Index (KDPI) now helps match kidneys to recipients. A low-KDPI kidney (under 20%) is from a young, healthy donor. A high-KDPI kidney (over 85%) might come from an older donor with high blood pressure. But here’s the key: even high-KDPI kidneys are better than staying on dialysis. Studies show they add years to your life.
Organ preservation has improved too. Machines that keep kidneys alive and beating outside the body-instead of just freezing them-are becoming more common. That means better function after transplant.
And the future? Scientists are working on tolerance-inducing therapies. The goal: teach your body to accept the new kidney without lifelong drugs. Clinical trials at Stanford and the University of Minnesota are testing ways to do this. If it works, transplant recipients might one day stop taking immunosuppressants altogether.
What If the Transplant Fails?
Transplants don’t last forever. The average lifespan of a living donor kidney is 15-20 years. Deceased donor kidneys last 10-15 years. When it fails, you go back to dialysis. That’s not a failure of you-it’s just how the body works.
Many people get a second transplant. You can be re-listed. And if you’re still healthy, you’ll likely do even better the second time around.
Can You Live a Normal Life After?
Yes. Most people return to work, travel, exercise, and even have children. You’ll need to avoid crowds during flu season, wash your hands often, and skip raw sushi or undercooked meat. But you can hug your grandkids, go on vacation, and enjoy meals without strict sodium limits.
One thing stays the same: you’ll always need to be your own advocate. Know your meds. Know your numbers. Know when to call your team. The transplant doesn’t fix everything-it gives you a second chance. And how you use it? That’s up to you.


Bryan Fracchia
January 27, 2026 AT 20:07People think it’s just medicine. Nah. It’s a second shot at being human again.
Kevin Kennett
January 28, 2026 AT 23:31Rose Palmer
January 29, 2026 AT 20:03Howard Esakov
January 30, 2026 AT 22:18Lexi Karuzis
January 31, 2026 AT 07:41Ambrose Curtis
February 1, 2026 AT 15:31Linda O'neil
February 1, 2026 AT 16:37Chris Urdilas
February 1, 2026 AT 18:30Jeffrey Carroll
February 2, 2026 AT 00:02