Why Your Medications Expire Sooner Than They Should
You bought that prescription for $40, took it home, and tossed it into the bathroom cabinet. A few months later, you find it tucked behind the toothpaste-still sealed, still labeled, but now marked expired. You throw it out, frustrated. But here’s the truth: it didn’t expire because time ran out. It expired because of how you stored it.
The FDA requires drugmakers to test their products under real-world conditions to set expiration dates. These dates aren’t arbitrary. They’re the last day the medication is guaranteed to work as intended-holding 90% to 110% of its labeled strength. But that guarantee only lasts if the drug stayed in the right environment. Most people don’t realize that humidity, heat, and light are the real killers of medicine, not time.
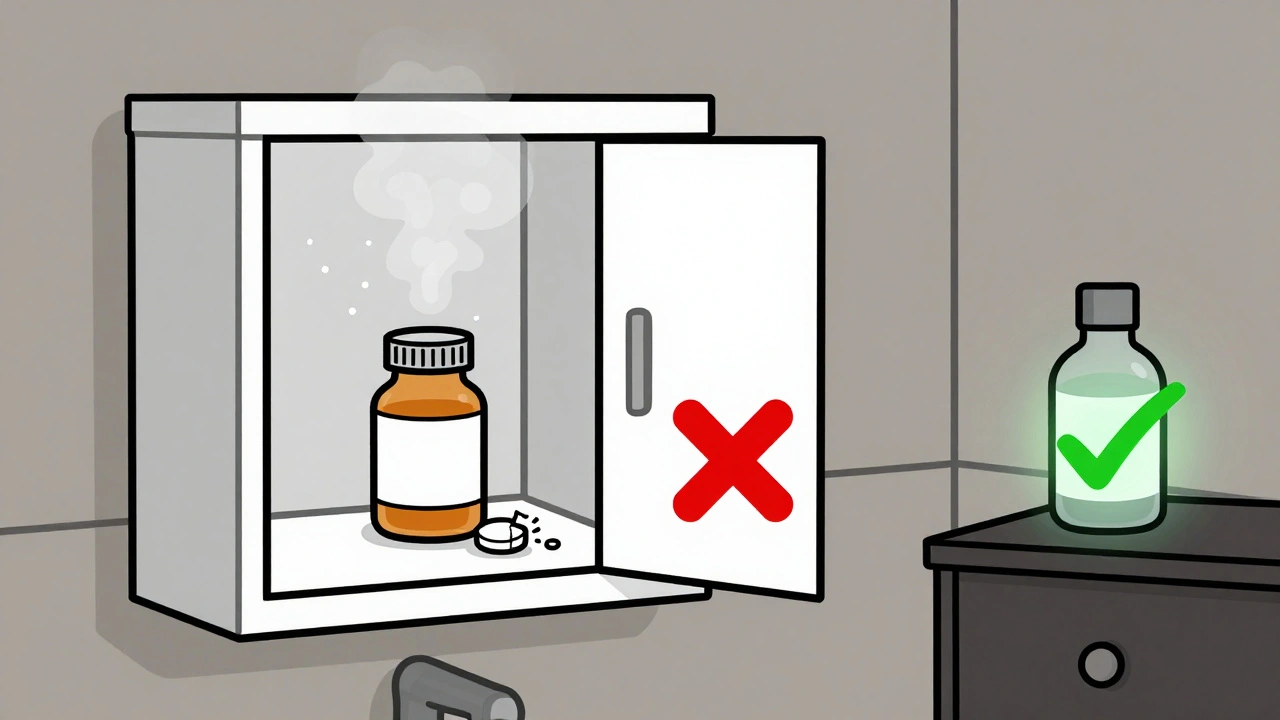
According to the CDC, 37% of premature medication expiration in homes comes from improper storage. And the biggest culprit? The bathroom. That warm, steamy room where you brush your teeth is the worst place to keep pills. During a hot shower, humidity spikes to 85-95%. That’s enough to break down aspirin three times faster than in dry air. Antibiotics stored near the stove lose potency in under three months. And if you’re keeping insulin in the fridge door? It’s getting hit with temperature swings every time someone opens it. That’s not storage-that’s sabotage.
What the Experts Say About Proper Storage
The U.S. Pharmacopeia (USP) and FDA agree: most tablets and capsules need to stay between 68°F and 77°F (20-25°C) with humidity below 60%. That’s not a suggestion. That’s science. Liquid medications like eye drops, insulin, and antibiotics often need refrigeration-but not just anywhere in the fridge. The door gets too warm. The back wall gets too cold. The center shelf? That’s the sweet spot: 36-46°F (2-8°C).
Some drugs have special rules. Nitroglycerin tablets? They must stay in their original dark glass bottle. Light turns them useless in minutes. Insulin? Once opened, it can sit at room temperature for up to 28 days-but only if it hasn’t been exposed to extreme heat. Merck’s new heat-stable insulin, approved in December 2023, can handle 86°F for 56 days. But that’s the exception, not the rule.
And don’t forget the bottle. Original prescription containers aren’t just for labeling-they’re designed to protect. Amber glass blocks 97% of UV light. Clear plastic? It lets in almost all of it. That’s why you shouldn’t transfer pills to a pill organizer unless you’re using it for daily doses and putting the rest back in the original bottle.
Where NOT to Store Your Medications
- Bathroom cabinets: Steam from showers raises humidity to dangerous levels. Aspirin breaks down faster here than anywhere else in the house.
- Kitchen counters near the stove or oven: Heat fluctuates wildly. One study found 42% of antibiotics degraded within 90 days in this environment.
- Car glove compartments: In summer, temperatures can hit 140°F. Even a few hours can ruin insulin, thyroid meds, or antidepressants.
- Under the sink: Moisture builds up. Mold grows. Pills get damp. Never store meds where water pipes run.
- On a windowsill: Sunlight degrades most medications. Even indirect light over weeks can reduce potency.
These aren’t myths. These are lab-tested facts. UCHealth’s 2023 study showed aspirin in a bathroom cabinet lost 30% of its potency in just six months. That’s not a little less effective-it’s not working as intended.
Where You SHOULD Store Your Medications
Find a cool, dry, dark spot. A bedroom dresser drawer is ideal. A locked cabinet in a closet works too. The key is consistency. Temperature should stay between 68-77°F. Humidity below 60%. No direct sunlight. No drafts.
For extra protection, use a small hygrometer (a humidity monitor) in the storage area. You can buy one for under $10 online. If it reads above 60%, add a silica gel packet-those little packets that come in new shoeboxes. They’re safe, non-toxic, and absorb moisture. Don’t use rice. It doesn’t work as well and can attract bugs.
Keep everything in its original container. That label has critical info: expiration date, storage instructions, lot number. If you need to use a pill organizer, only fill it with what you’ll take that day. Then return the rest to the original bottle.
And if you have kids or pets? Lock it up. The American Association of Poison Control Centers reports over 100,000 accidental pediatric medication exposures each year. A simple lockbox makes all the difference.
How to Spot Degraded Medication
Just because a pill hasn’t passed its expiration date doesn’t mean it’s still good. Look for these warning signs:
- Odor: Aspirin that smells like vinegar? It’s broken down into acetic acid. Toss it.
- Color change: If a white tablet is now yellow, brown, or spotted, it’s degraded. Same with capsules that have stuck together or leaked.
- Texture: Tablets that crumble easily or feel sticky? That’s moisture damage.
- Cloudiness or particles: Liquid meds like eye drops or insulin should be clear. If you see flakes, strings, or cloudiness, don’t use them. The CDC warns that contaminated eye drops can cause serious eye infections like bacterial conjunctivitis.
When in doubt, throw it out. Taking a degraded medication isn’t just ineffective-it can be dangerous. A study in the New England Journal of Medicine found that degraded tetracycline can cause kidney damage. That’s not a risk worth taking.
Organize and Track to Avoid Waste
One of the biggest reasons meds expire early? No one checks them. A Kaiser Permanente study found that assigning one person in the household to do a monthly expiration check cuts premature disposal by 89%. That’s huge.
Try this simple system:
- Take out all your meds once a month.
- Check each bottle’s expiration date.
- Use colored dot stickers: red for this year, blue for next year, green for two years out.
- Put anything expiring in the next 60 days on your calendar to refill or replace.
This method was tested at the University of Wisconsin-Madison and reduced expired meds by 63% in just six months. It’s not fancy. It’s just consistent.
Smart pillboxes like the MedMinder Pro now monitor temperature and humidity inside the device. If your meds are getting too hot or damp, it sends an alert to your phone. They cost around $150, but for high-cost or life-saving drugs, it’s worth it.

What to Do With Expired or Unused Medications
Never flush pills down the toilet. The CDC says 55% of households still do this, polluting waterways and harming wildlife. Don’t toss them in the trash either-someone could find them.
Use a drug take-back program. The DEA runs National Prescription Drug Take Back Day twice a year. The next one is October 26, 2024. Over 11,000 collection sites across the U.S. accept all types of meds-pills, liquids, patches, even needles. Find your nearest site at dea.gov/takeback.
Some pharmacies offer year-round drop-off bins. Check with your local CVS, Walgreens, or independent pharmacy. If no take-back is available, mix pills with coffee grounds or cat litter in a sealed bag before throwing them out. That makes them unappealing and unusable.
What’s Changing in Medication Storage
The industry is catching up. Since 2024, 78% of new prescription labels include simple icons showing storage needs: a snowflake for refrigeration, a sun with a slash for avoiding light, a thermometer for temperature ranges.
Merck’s new heat-stable insulin is just the beginning. The FDA is working on rules to require real-time stability indicators on high-risk drugs-think color-changing labels that show if the drug has been exposed to bad conditions.
And researchers at the University of Wisconsin are testing prescription bottles with built-in silica gel. Early results show they keep humidity 45% lower than standard bottles. If approved, they’ll be a game-changer.
Meanwhile, community campaigns like the American Pharmacists Association’s “Store It Safe” have reached over 1.2 million households since 2022. In those areas, premature expiration dropped by 27%.
Final Tip: Don’t Guess. Check.
You don’t need to be a pharmacist to keep your meds safe. You just need to know where to put them, how to check them, and when to toss them. Medications aren’t like wine-they don’t get better with age. They get weaker. And when they do, your health pays the price.
So next time you reach for that bottle, ask yourself: Is this where it’s supposed to be? Is it still clear? Does it smell right? If not, don’t risk it. Get a new one. Your body will thank you.
Can I still use medicine after the expiration date?
The expiration date is the last day the manufacturer guarantees full potency and safety. Most medications don’t suddenly become toxic after that date, but they lose effectiveness. For non-critical drugs like pain relievers, using them a few months past expiration might be low-risk-but not for antibiotics, heart meds, insulin, or epinephrine. Those can fail when you need them most. Never use expired life-saving drugs.
Is it safe to store pills in the refrigerator?
Only if the label says to. Most pills don’t need refrigeration and can be damaged by moisture. But liquids like insulin, eye drops, and some antibiotics must be kept cold. Store them in the center of the fridge, not the door. Always keep them in their original container to protect from condensation.
Why do some medications need to be kept in the dark?
Light, especially UV rays, breaks down certain chemicals in medications. Nitroglycerin, for example, becomes useless if exposed to light. That’s why it comes in dark glass bottles. Other drugs like tetracycline and certain antidepressants can also degrade under light. Always keep them in their original container, which is designed to block harmful rays.
How do I know if my liquid medicine has gone bad?
Look for cloudiness, particles, or color changes. If it smells funny or has a strange texture-like it’s thicker or thinner than usual-don’t use it. Eye drops and insulin are especially risky. Contaminated eye drops can cause serious eye infections. If you’re unsure, throw it out and get a new prescription.
What’s the best way to dispose of old medications?
Use a drug take-back program. The DEA hosts collection events twice a year, and many pharmacies have year-round drop boxes. If neither is available, mix pills with coffee grounds or cat litter in a sealed plastic bag before tossing them in the trash. Never flush them. It pollutes water and can harm wildlife.




Stacy here
December 7, 2025 AT 18:47Ryan Sullivan
December 8, 2025 AT 06:10Helen Maples
December 8, 2025 AT 15:24Ashley Farmer
December 9, 2025 AT 00:43Sadie Nastor
December 9, 2025 AT 05:06Sangram Lavte
December 10, 2025 AT 04:14Oliver Damon
December 11, 2025 AT 18:46