By 2025, the world will spend over $1.6 trillion on medicines. That’s more than the entire GDP of Canada. And yet, billions of people still pay for their drugs out of their own pockets-sometimes selling livestock or skipping meals to afford insulin or blood pressure pills. The reason this doesn’t spiral into total collapse? Generics.
Generics Are the Hidden Backbone of Global Health
When you hear "pharmaceuticals," you think of flashy new drugs with billion-dollar price tags. But in reality, 80 to 90% of all prescriptions filled in the U.S., Europe, and Japan are generics. These are the same drugs as the brand-name versions-same active ingredients, same effectiveness, same safety standards-but they cost 80% less. In India, Brazil, and South Africa, generics make up over 95% of the market. Without them, global healthcare systems would collapse under the weight of innovation-driven pricing.
The math is simple: a brand-name cancer drug might cost $10,000 a month. The generic version? $2,000. That’s not a small saving-it’s the difference between life and death for families in middle-income countries. In Nigeria, where the average person earns less than $2,000 a year, a $10,000 drug might as well be science fiction. But a $2,000 generic? That’s something a community clinic can stock.
Why Drug Prices Keep Rising-And Why Generics Can’t Always Stop It
It’s true: global drug spending is still climbing. In the U.S., prescription drug costs jumped $50 billion in 2024 alone. But here’s what you won’t hear in headlines: most of that growth isn’t from generics. It’s from specialty drugs-new treatments for rare cancers, autoimmune diseases, obesity, and diabetes. These aren’t pills you can copy. They’re complex biologics, made from living cells, requiring years of research and billions in investment. That’s why they’re expensive.
Even when generics enter the market, they don’t always replace the brand. In the U.S., doctors often stick with the brand because of insurance formularies, patient loyalty, or marketing pressure. In Europe, some countries have strict rules about switching patients from brand to generic without consent. In places like Turkmenistan or Afghanistan, where healthcare systems are barely functional, generics may be available-but there’s no supply chain to deliver them.
Meanwhile, biosimilars-generic versions of biologic drugs-are starting to appear. But adoption is slow. In the U.S., only 1 in 5 biologics have a biosimilar available. In low-income countries, they’re often not even registered. Regulatory hurdles, lack of local manufacturing, and physician resistance all hold them back.

The Real Cost of Not Using Generics
When countries skip generics, the consequences show up in hospitals, not balance sheets.
Lebanon’s public health spending dropped 71% between 2019 and 2021. Malawi’s fell 41%. In both places, the only reason people still got their HIV meds or hypertension pills was because generic versions were available through global aid programs. When those generics were delayed due to import issues, deaths spiked. That’s not speculation-it’s documented by the WHO.
And it’s not just poor countries. In the U.S., out-of-pocket spending on prescriptions is projected to rise from $177 per person in 2025 to $231 by 2033. That’s a 30% increase. For a diabetic on insulin, that could mean choosing between medicine and rent. Generics could cut that burden in half. But only if they’re accessible.
Insurance companies know this. A 2025 survey of 200+ insurers worldwide found that 67% expect demand for healthcare services to rise sharply in the next three years. Mental health alone is projected to see a 15%+ cost spike per person. Generic antidepressants and antipsychotics are the only affordable way to meet that demand.
Where Generics Are Winning-and Where They’re Losing
Not all countries are the same. In Germany, generics account for 70% of prescriptions by volume and 30% of spending. That’s because the government forces pharmacies to dispense the cheapest option unless the doctor writes "do not substitute." In the U.K., the NHS saves over £1 billion a year just by switching to generics.
But in the U.S., the system is broken. Patents are extended. Pay-for-delay deals let brand-name companies pay generic makers to stay off the market. The result? A new heart drug might have a generic version ready-but it won’t hit shelves for another two years. Meanwhile, patients pay $500 a month for a pill that could cost $20.
In emerging markets, the story is different. China is shifting from being a cheap generic producer to becoming a major buyer of new drugs. As incomes rise, so does demand for branded treatments. That’s good for innovation-but bad for affordability. If China follows the U.S. model, billions could be priced out of care.
The Future of Generics: More Than Just Cheap Pills
Generics aren’t just about price. They’re about access, equity, and system sustainability. As global health spending grows, and as climate change and aging populations strain systems, the role of generics will become even more critical.
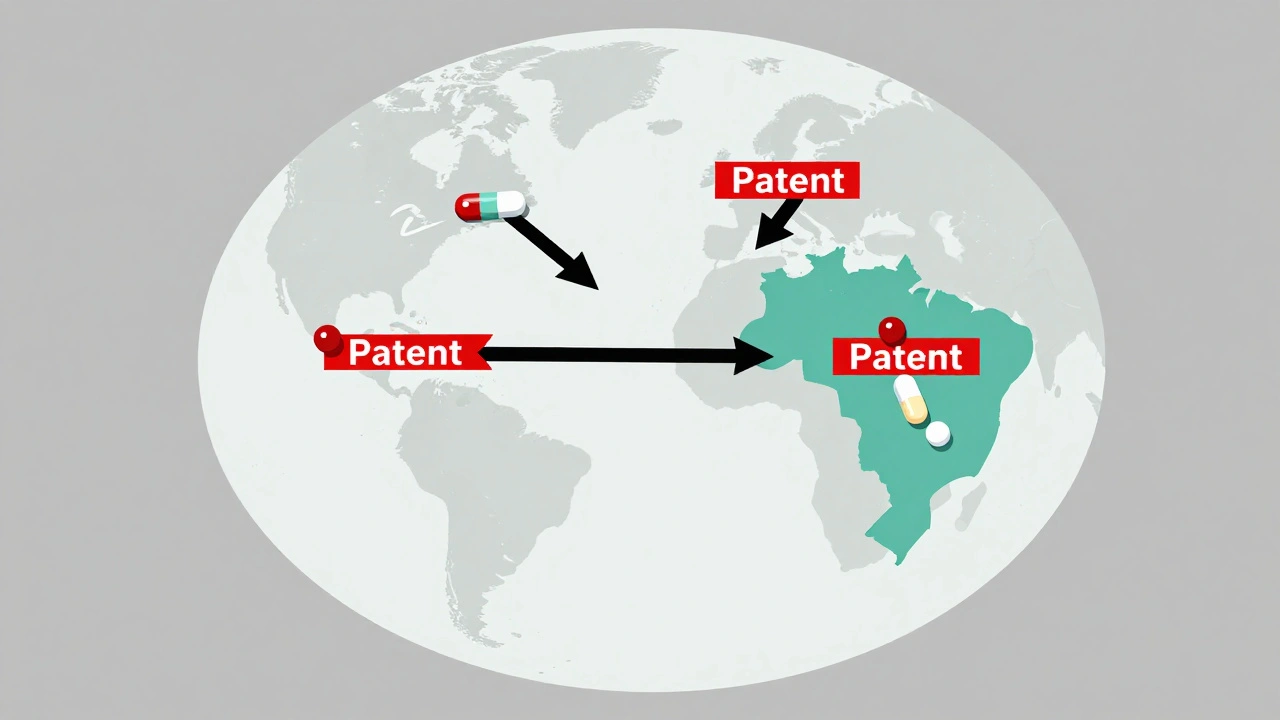
By 2030, the world will need 10 million more healthcare workers. But even if we had them, we couldn’t afford to treat everyone with expensive drugs. That’s why the WHO and the World Bank are pushing for generic procurement programs. Why India and Brazil are investing in local generic manufacturing. Why countries like Thailand and South Africa are using compulsory licensing to produce their own versions of life-saving drugs.
The next big wave isn’t just about more generics. It’s about smarter generics. Biosimilars that work as well as the original. Generic versions of combination pills that simplify treatment. Digital tools that track generic supply chains so no clinic runs out of antibiotics.
And yet, the biggest barrier isn’t technology. It’s politics. Drug companies spend billions lobbying against generic competition. Governments fear losing tax revenue from branded drugs. Pharmacies profit more from selling expensive brands.
What Needs to Change
Here’s what actually works:
- Force automatic substitution. Countries like Sweden and the Netherlands require pharmacists to give the cheapest option unless the doctor says no. That cuts costs fast.
- Stop pay-for-delay deals. The U.S. FTC has sued drug companies for these shady contracts. More enforcement is needed.
- Invest in local generic production. Africa imports 90% of its medicines. Building regional manufacturing hubs in Nigeria, Kenya, and Ethiopia could cut prices by half.
- Expand generic access in humanitarian crises. When war hits, aid groups bring in branded drugs. They should be mandated to use generics unless absolutely necessary.
- Teach doctors and patients. Many still believe generics are "inferior." They’re not. They’re the same drug, just cheaper.
The bottom line? Generics aren’t a side note in global health. They’re the foundation. Without them, universal healthcare is just a slogan. With them, even the poorest country can treat hypertension, diabetes, depression, and infections.
It’s not about choosing between innovation and affordability. It’s about making sure innovation doesn’t leave the world behind.
Are generic drugs really as effective as brand-name drugs?
Yes. Generic drugs must meet the same strict standards as brand-name drugs. They contain the same active ingredients, work the same way, and are tested for safety and effectiveness. The only differences are in the inactive ingredients-like fillers or coatings-which don’t affect how the drug works. The U.S. FDA and the European Medicines Agency require generics to be bioequivalent, meaning they deliver the same amount of medicine into the bloodstream at the same rate as the brand.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to repeat the expensive clinical trials that brand-name companies do. Once a patent expires, multiple companies can make the drug, creating competition. That drives prices down. Brand-name companies spend billions on research, marketing, and patents. Generics only pay for production and regulatory approval-so their costs are far lower.
Do all countries use generics the same way?
No. High-income countries like Germany and the U.K. use generics heavily because their systems encourage it-through policy, reimbursement rules, and pharmacist substitution. In the U.S., use is lower due to patent extensions, insurance incentives, and doctor habits. In low-income countries, generics are often the only option-but supply chains are weak, and quality control can be inconsistent. Some countries, like India and Brazil, are major producers, while others rely entirely on imports.
What’s the difference between generics and biosimilars?
Generics are exact copies of small-molecule drugs, like aspirin or metformin. Biosimilars are similar-but not identical-to complex biologic drugs made from living cells, like insulin or Humira. Because biologics are made by living organisms, they can’t be copied exactly. Biosimilars must be shown to work just as well and be just as safe, but they’re harder to produce and more expensive than traditional generics. That’s why adoption is slower.
Can generics help reduce out-of-pocket costs for patients?
Absolutely. In the U.S., switching from a brand-name drug to its generic can cut a patient’s monthly cost from $300 to $30. In Nigeria, a generic version of an HIV drug costs less than $1 per month, while the brand might cost $100. For millions of people without insurance, generics are the only reason they can afford treatment. Without them, many would simply stop taking their medicine.
Why don’t all doctors prescribe generics?
Some doctors are used to prescribing brands because of training, marketing, or habit. Others worry patients will think generics are "inferior," even though that’s not true. In some countries, insurance plans pay doctors more to prescribe branded drugs. And in the U.S., pharmaceutical companies spend over $6 billion a year on direct-to-consumer ads for brand-name drugs, shaping patient expectations. But when patients ask for generics, most doctors will switch-if the system lets them.
Are there risks with using generics?
When approved by reputable regulators like the FDA, EMA, or WHO, generics are just as safe as brand-name drugs. But in countries with weak oversight, counterfeit or substandard generics do exist. That’s why it’s critical to source generics through official channels. The WHO’s Prequalification Program helps ensure quality in low-income countries. If you’re buying online or from unlicensed vendors, there’s risk-but that’s true for any medicine, branded or generic.
How do generics affect global health equity?
Generics are one of the most powerful tools for health equity. In 2022, no low-income country spent more than 1.2% of its GDP on healthcare. Without generics, many couldn’t afford even basic treatments. For example, generic antiretrovirals made HIV treatment possible across Africa. Generic antibiotics saved millions in low-income countries during the pandemic. When countries can’t afford expensive drugs, generics are the bridge to basic care.



Michael Robinson
December 10, 2025 AT 04:25Generics are the quiet heroes of medicine. No one throws them parades, but they keep millions alive. It’s not magic-it’s just math. Same molecule, same effect, 80% cheaper. Why do we act like it’s a compromise? It’s not. It’s common sense.
Andrea Petrov
December 11, 2025 AT 14:48Did you know the FDA allows generics to vary by up to 20% in absorption? That’s not a typo. That’s why some people feel ‘different’ on generics-it’s not placebo, it’s chemistry. Big Pharma knows this. That’s why they push brand loyalty. They’re not selling pills. They’re selling control.
Suzanne Johnston
December 12, 2025 AT 07:12I’ve worked in NHS pharmacies for 22 years. I’ve seen patients cry because they couldn’t afford their insulin. Then the generic came in. Same pill. Same results. But now they could pay for groceries too. It’s not about politics. It’s about dignity. When you force a person to choose between medicine and bread, you’ve already lost the moral high ground.
Germany doesn’t have this problem because they don’t let marketing dictate prescriptions. Pharmacists dispense the cheapest. End of story. We should be doing the same. Not because it’s cheap-but because it’s right.
Graham Abbas
December 12, 2025 AT 21:33Let me tell you about my cousin in Manchester. She’s on a biologic for rheumatoid arthritis. Cost? £1,800 a month. The biosimilar? £400. She switched. Her pain didn’t change. Her rent didn’t go up. Her mental health improved because she stopped worrying about bills. And yet-her doctor never even mentioned the biosimilar. Why? Because no one’s trained to think about cost. We’re trained to think about brands. That’s the real disease.
Haley P Law
December 13, 2025 AT 06:04OMG I JUST REALIZED MY ANTIDEPRESSANT IS A GENERIC 😭 I THOUGHT I WAS ON THE ‘PREMIUM’ ONE 😅 I’M STILL FUNCTIONING??!!?? I’M NOT CRAZY??!!?? 🙏🙏🙏
Andrea DeWinter
December 15, 2025 AT 05:43People think generics are inferior because they’re cheaper but that’s like saying a Honda Civic is worse than a BMW because it costs less. Same roads same rules same engine. Just no leather seats. The FDA doesn’t cut corners. If it’s approved it works. Stop letting pharma scare you into paying more. Your body doesn’t care about the logo.
ian septian
December 15, 2025 AT 22:49Generics save lives. That’s it.
Arun Kumar Raut
December 16, 2025 AT 00:29I work in a clinic in Mumbai. We give out generic HIV meds. Cost per patient per month: 30 rupees. That’s less than a cup of chai. Last year, we had 200 new patients. All alive. All working. All feeding their kids. The brand version? 3,000 rupees. Impossible. We don’t have a choice. But we shouldn’t have to make one. Generics aren’t a Band-Aid. They’re the foundation. And India makes them. We should be proud.
When I see Westerners debate this like it’s a luxury, I want to scream. You don’t get to choose between life and rent. We live it every day.
precious amzy
December 17, 2025 AT 12:18One must interrogate the epistemological foundations of the generic paradigm. The very notion that bioequivalence constitutes therapeutic equivalence is a reductive positivist fallacy. The ontological integrity of the pharmaceutical object is compromised by its commodification. One cannot reduce the phenomenological experience of illness to a pharmacokinetic curve. The corporate hegemony of the generic industry, while ostensibly egalitarian, in fact perpetuates a homogenized, depersonalized medical ethos. One must ask: is accessibility truly liberation, or merely the quiet surrender of therapeutic nuance?