Chronic eczema isn’t just dry skin. It’s a broken barrier, a runaway itch, and a cycle that feels impossible to break. If you’ve been dealing with this for months or years, you know it’s not about moisturizing more. It’s about fixing what’s broken inside your skin - and doing it right.
Why Your Skin Barrier Is the Root Problem
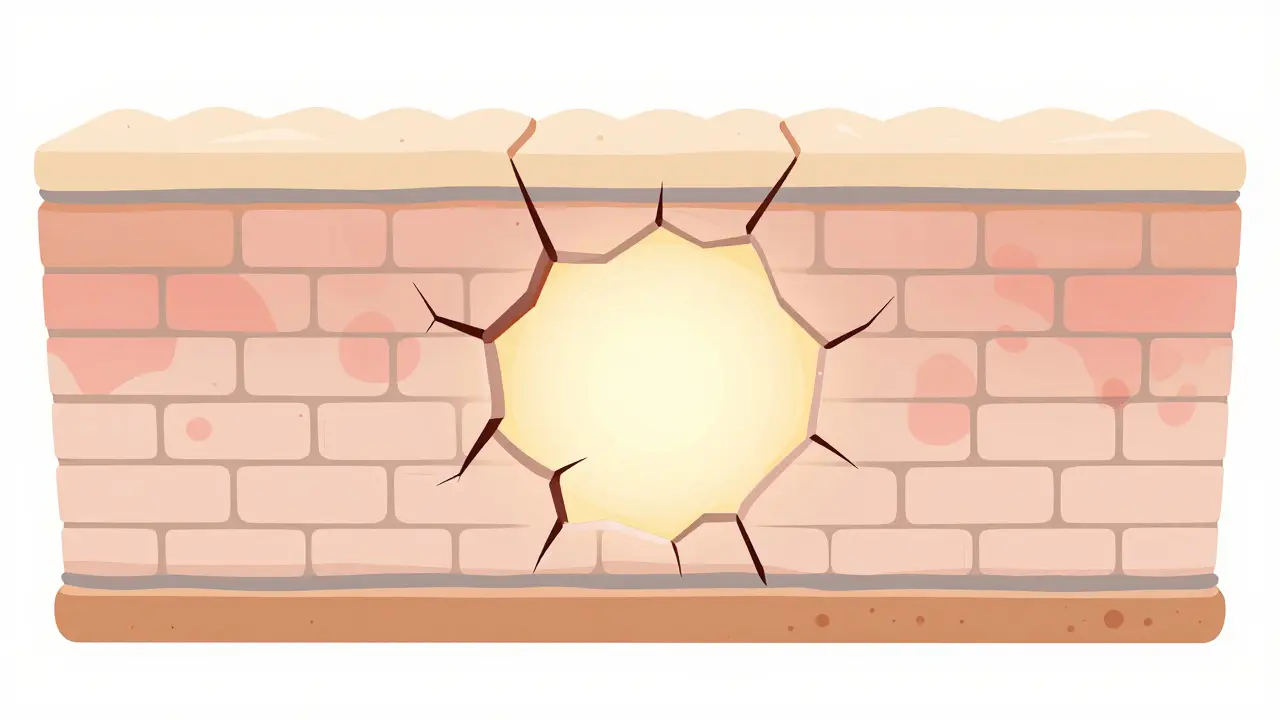
Your skin isn’t just a surface. It’s a layered defense system. The outermost layer, called the stratum corneum, acts like a brick wall. The bricks are dead skin cells (corneocytes), and the mortar is made of lipids - ceramides, cholesterol, and fatty acids. In chronic eczema, that mortar is crumbling.Research shows this breakdown happens before any redness or itching shows up. In high-risk babies, the barrier fails 3 to 6 months before the first flare. That’s why simply treating the rash doesn’t work long-term. You’re fixing the symptom, not the cause.
Half of people with moderate to severe eczema have mutations in the filaggrin gene. This gene makes a protein that helps hold skin cells together and keeps moisture in. When it’s broken, your skin loses water fast - up to 40 grams per square meter per hour, compared to 8-12 in healthy skin. That’s why your skin feels tight, cracked, and raw.
On top of that, ceramide levels drop by 30-50%, especially ceramide 1, the one that forms the strongest lipid layers. What’s left are short-chain ceramides that don’t seal properly. Think of it like using the wrong kind of glue - it looks like it’s holding, but it falls apart under pressure.
Barrier Repair Isn’t Just Moisturizing - It’s Rebuilding
Most over-the-counter lotions? They’re just water with a little oil. They give temporary relief, but they don’t fix the structure.True barrier repair products use a specific recipe: ceramides, cholesterol, and free fatty acids in a 1:1:1 ratio. That’s not random. That’s what healthy skin naturally contains. Clinical trials show these formulations restore the barrier 87% of the time, compared to 52% with basic petrolatum or glycerin creams.
Look for products with 3-5% ceramides, 2-4% cholesterol, and 1-3% free fatty acids. Brands like CeraVe, EpiCeram, and Atopiclair use this formula. You’ll pay more - around $28 for 200g versus $10 for a basic cream - but you’re buying science, not just hydration.
And don’t ignore pH. Your skin’s natural pH is 4.5-5.5. If your cream is too alkaline (like many soaps), it shuts down an enzyme called β-glucocerebrosidase that’s essential for making ceramides. At pH 7, it works at 40% efficiency. At pH 5, it’s at 90%. That’s why some barrier creams feel slightly acidic on the skin - they’re designed to work with your body, not against it.
What Makes Your Eczema Flare Up (And How to Avoid It)
Triggers aren’t the same for everyone, but some show up again and again.Harsh soaps and hot showers - They strip away the last of your natural oils. Water hotter than 100°F (38°C) damages the barrier. Stick to lukewarm water and use fragrance-free cleansers like Cetaphil or Vanicream.
Dry air - Especially in winter. Indoor heating drops humidity to 20-30%. Use a humidifier in your bedroom. Keep it at 40-50% humidity. It’s not luxury - it’s medical.
Sweat - Salt and ammonia in sweat irritate broken skin. Wash off after exercise. Pat dry - don’t rub.
Stress - It doesn’t cause eczema, but it turns up the volume on inflammation. Your body releases cortisol and other chemicals that worsen itching. Meditation, deep breathing, or even 10 minutes of walking daily can help.
Staphylococcus aureus - This bacteria loves eczema skin. It colonizes cracks, releases toxins, and triggers more inflammation. Barrier repair reduces its presence by 65-75%. That’s why healing the barrier is your first line of defense - it makes your skin less inviting to bugs.
Food allergies - Only a small group (about 10-30%) of adults with eczema have food triggers. Don’t eliminate foods without testing. If you suspect a link, talk to an allergist, not your Instagram feed.

How to Break the Itch-Scratch Cycle
Itch is the worst part. It’s not just annoying - it’s exhausting. Scratching doesn’t just damage skin - it makes inflammation worse. It’s a loop: itch → scratch → inflammation → more itch.Here’s how to stop it:
- Cool compresses - Damp, cool (not icy) cloth on the itch for 5-10 minutes. It numbs the nerve endings.
- Wet wrap therapy - Apply moisturizer, then cover with damp cotton clothing or gauze, then a dry layer. Do this at night. Studies show it cuts itching by 70% in 7 days.
- Topical calcineurin inhibitors - Pimecrolimus or tacrolimus creams. They don’t thin skin like steroids, and they reduce itching without sedation. Use them on face, neck, and folds - areas where steroids are risky.
- Oral antihistamines - They don’t stop the itch from eczema (it’s not histamine-driven), but they help you sleep. Diphenhydramine or hydroxyzine at night can break the sleep-itch cycle.
- Behavioral tricks - Keep your nails short. Wear cotton gloves at night. When you feel the itch, tap the area instead of scratching. It sends a different signal to your brain.
One user on Reddit tracked their itch for 30 days. After switching to a ceramide cream and using wet wraps, nighttime scratching dropped from 5-6 times a night to 1-2. They said, “I actually slept through the night for the first time in years.”
When Barrier Repair Alone Isn’t Enough
For some, especially those with severe filaggrin mutations, barrier repair helps - but doesn’t fix everything. When TEWL (water loss) stays above 45 g/m²/h, you need more.Topical steroids like betamethasone work fast - reducing TEWL by 35% in a week. But they thin the skin over time. That’s why they’re for short bursts, not daily use.
For persistent cases, doctors now turn to JAK inhibitors (like upadacitinib or abrocitinib). These oral pills block the inflammation signals that keep eczema going. They’re not first-line, but they’re life-changing for those who’ve tried everything else.
And new options are coming. Platelet-rich plasma (PRP) injections are being tested to boost filaggrin production. Early data shows a 300% increase in filaggrin expression after treatment. It’s experimental, but promising.
Genetic testing is also becoming part of care. Companies like Dermavant are using 23andMe data to match patients with barrier creams based on their filaggrin mutation. If you have a null mutation, you’ll need stronger support - and you’ll know it sooner.
How to Use Barrier Creams Right (So They Actually Work)
You can have the best cream in the world, but if you use it wrong, it won’t help.- Apply within 3 minutes of bathing - That’s when your skin is still holding water. Waiting 10 minutes cuts effectiveness by 35%.
- Use enough - For both arms, use 5 grams - that’s about two fingertip units (the amount from the tip of your finger to the first joint). Most people use half that.
- Apply twice daily - Morning and night. Even if your skin looks fine.
- Don’t mix with steroids - Apply steroid first, wait 15 minutes, then apply barrier cream. Applying them together reduces the cream’s absorption.
- Be patient - It takes 28-42 days to rebuild the barrier. Don’t quit after a week. You’re not failing - you’re just not done yet.
One study found 92% compliance was needed to see real TEWL improvement. That means you have to use it almost every day. If you miss two days a week, you’re not getting the full benefit.
Cost, Compliance, and Real-World Challenges
The biggest reason barrier repair fails? People stop using it.Forty percent say the creams feel too greasy. Others say they sting at first - especially on broken skin. That’s normal. It usually fades after 3-5 days. If it burns for more than a week, switch brands.
Cost is a barrier. Insurance covers prescription barrier creams like EpiCeram 80% of the time. But over-the-counter ones? Medicare pays only 30%. That’s why many people go back to cheap petrolatum - even though it doesn’t fix the root problem.
But here’s the math: One flare can cost $200 in doctor visits, prescriptions, and missed work. A $30 cream that cuts flares by half? That’s a bargain.
Community support helps. Reddit’s r/Eczema has over 12,500 members sharing tips. MyEczemaTeam has 500+ video tutorials on application techniques. Watching someone do it right - not just reading about it - increases adherence by 30%.
What’s Next for Eczema Treatment
The future is personal. By 2030, barrier repair could make up half of all eczema care. Why? Because we’re finally treating the cause, not just the symptoms.New formulations are coming - biodegradable bases to meet EU regulations, nano-ceramides that penetrate deeper, and even probiotic sprays to restore the skin’s microbiome.
And the biggest shift? Doctors are no longer asking, “What’s causing your flare?” They’re asking, “What’s broken in your barrier?”
It’s not magic. It’s biology. And it’s working.
Can barrier repair cure chronic eczema?
No, barrier repair doesn’t cure eczema - but it can put it into long-term remission. For many, consistent use reduces flares from weekly to monthly or less. In children, early barrier repair can even prevent eczema from becoming severe. It’s the most effective long-term strategy we have.
How long does it take to see results from ceramide creams?
Most people notice less dryness and less itching within 2 weeks. But full barrier repair takes 4-6 weeks. Clinical studies show TEWL improves significantly after 28 days. Don’t judge it before then.
Are expensive barrier creams worth it over drugstore lotions?
Yes - if they contain the right lipids. A $10 lotion with just glycerin and mineral oil won’t fix your barrier. A $30 cream with 3% ceramides, 2% cholesterol, and 1% fatty acids in a 1:1:1 ratio will. Look at the ingredient list, not the price tag. Brands like CeraVe and EpiCeram have proven formulas.
Can I use barrier cream with steroid ointments?
Yes, but not at the same time. Apply the steroid first, wait 15 minutes, then apply the barrier cream. Mixing them reduces the cream’s ability to repair. The National Eczema Association recommends this timing for best results.
Why does my barrier cream sting when I apply it?
It’s common, especially on cracked or inflamed skin. Barrier creams are often slightly acidic (pH 5-5.5) to support enzyme function, and that can sting on open areas. The sting should fade after 3-5 days. If it burns continuously or gets worse, stop and switch to a gentler formula.
Is eczema linked to gut health or diet?
There’s no strong evidence that diet causes eczema in adults. Some children may have food triggers, but eliminating foods without testing can lead to nutritional gaps. Focus on skin barrier repair first. If flares persist, consult an allergist - don’t guess.
If you’ve tried everything and still feel stuck, remember: you’re not failing. Your skin is just asking for the right tools. Barrier repair isn’t glamorous - but it’s the most powerful thing you can do.


Jenci Spradlin
January 8, 2026 AT 01:12bro i was using ceraVe for months and it did nothing until i switched to the one with the 1:1:1 ratio. i didnt even know that was a thing. my skin stopped cracking after 3 weeks. also dont wash with hot water like i did for 5 years lmao.
Johanna Baxter
January 9, 2026 AT 23:29so basically its all just a scam to sell you expensive creams? i bet the real cause is your mom didn’t love you enough. or maybe your wifi router is giving you eczema. i’ve been living in a cave for 12 years and my skin is perfect. you’re all just weak.
Patty Walters
January 10, 2026 AT 10:22the sting thing is real. first time i used a ceramide cream it burned like hell. i thought i was gonna have to go to the er. but i stuck with it for 4 days and now it feels like a hug for my skin. also wet wraps at night? game changer. i used to wake up with bloody arms. now i just wake up and remember what sleep is.
Phil Kemling
January 10, 2026 AT 20:22the real tragedy isn’t the broken barrier-it’s that we’ve been conditioned to treat symptoms as problems, rather than signals. we medicate the itch, not the silence between the bricks. the skin isn’t failing-it’s screaming for coherence. and yet, we offer it lotion like a pacifier. we don’t rebuild. we mask. and then we wonder why it keeps happening.
tali murah
January 11, 2026 AT 17:13Oh, so now it’s ‘science’? Let me guess-you also believe in the 1:1:1 ratio like it’s the holy trinity of dermatology. Meanwhile, people with actual jobs can’t afford $30 creams and are stuck with Vaseline. And you call that ‘medical advice’? What a privilege. Next you’ll tell me to meditate while my skin peels off in sheets.
Diana Stoyanova
January 13, 2026 AT 04:57OMG I’M SO GLAD I FOUND THIS!! I’ve been doing wet wraps for 2 weeks and I swear I’ve never slept this well in my life. Like, I actually REMEMBERED MY DREAMS. And my kid started using the ceramide cream and her flares went from daily to once a month?? I’m crying right now. You guys are my heroes. Also, I bought the EpiCeram and I’m literally hugging the tube. I’ve never loved a product this much. I even made a playlist called ‘Ceramide Dreams’ to play while I apply it. 🌿💤✨
Lindsey Wellmann
January 13, 2026 AT 19:05you’re all missing the point. the real issue is that society doesn’t value skin health. we’re taught to ignore pain, hustle through discomfort, and ‘just deal with it.’ but your skin? it remembers everything. every stress, every bad soap, every sleepless night. and it’s paying the price. so if you’re not treating your skin like a sacred temple… you’re not trying hard enough. 🕊️🧬
Jeffrey Hu
January 14, 2026 AT 17:28you forgot to mention that ceramide creams only work if you’re not using sodium lauryl sulfate in your shampoo. also, the 1:1:1 ratio is outdated-new studies show 3:2:1 is better for filaggrin-null mutations. and don’t even get me started on how most people misapply it. you need to press it in, not rub. and the 3-minute window? that’s only true if your skin is below 32°C. most people’s skin is warmer after a shower. so you’re all wrong. and yes, I read the journal articles.