Generic Medication Excipient Risk Checker
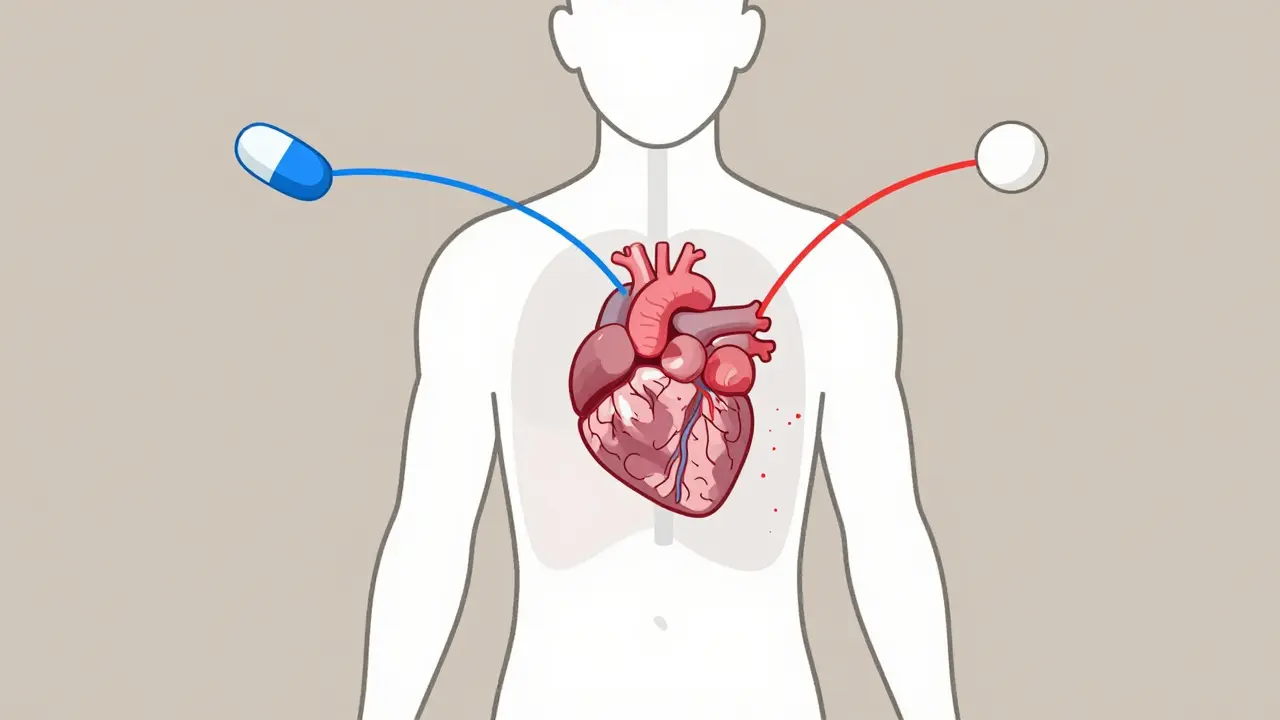
This tool helps you understand potential risks when switching to generic medications based on your sensitivities. The FDA requires generics to have the same active ingredient, but excipients (inactive ingredients) can differ and cause reactions for sensitive individuals.
When you pick up a prescription, you might not think twice about whether it’s the brand-name version or the generic. After all, the pill looks similar, the label says the same thing, and your co-pay is way lower. But here’s something most people don’t realize: the difference between brand and generic medications isn’t just in price-it’s often in what’s hidden inside.
Both brand and generic drugs contain the exact same active ingredient. That’s the part that actually treats your condition-whether it’s high blood pressure, epilepsy, or thyroid dysfunction. The FDA requires generics to match the brand in strength, dosage, and how quickly the drug gets into your bloodstream. So why do some people feel worse after switching? The answer lies in the inactive ingredients-what scientists call excipients.
What Are Excipients, Really?
Excipients are the non-active parts of a pill. They don’t cure anything. But they do a lot of important jobs: they hold the pill together, help it dissolve at the right speed, give it color, make it taste better, or keep it from falling apart in your medicine cabinet. Think of them like the scaffolding around a building. The building is the active drug. The scaffolding? That’s the excipient.
Here’s the catch: while the active ingredient must be identical, manufacturers of generic drugs can-and often do-use different excipients than the brand-name version. One generic version of a blood pressure pill might use cornstarch as a filler. Another might use lactose. One might be coated with a dye made from red #40. Another might use titanium dioxide. None of these change the drug’s effect… usually. But for some people, they change everything.
When Excipients Cause Real Problems
Most people switch to generics without a hitch. In fact, studies show that 92% of generic drugs perform just as well as their brand-name counterparts. But that 8%? They’re not just unlucky-they’re often people with hidden sensitivities.
Take lactose. It’s a common filler in pills. If you’re lactose intolerant, you might not even think about it. But if you’re taking a generic version of a heart medication that uses lactose as a binder, you could end up with bloating, cramps, or even diarrhea. Those symptoms? They don’t just make you uncomfortable. They can mess with how fast your body absorbs the drug. For someone on a narrow therapeutic index medication-like warfarin or levothyroxine-that small delay can mean the difference between your blood clotting safely and clotting dangerously.
There’s a documented case of a patient who developed a severe allergic reaction after switching from branded furosemide to a generic version. The culprit? Croscarmellose sodium, a disintegrant used to help the pill break down. The brand used a different compound. The patient had never reacted before-until the generic.
For Parkinson’s patients, this isn’t theoretical. A 2023 survey by the Michael J. Fox Foundation found that 18% of 5,247 patients reported worse symptoms after switching from branded levodopa to a generic version. One Reddit user wrote: “I went from having 2 ‘off’ periods a day to 6. My hands shook so bad I couldn’t hold a coffee cup.” The change? A different binder in the generic capsule altered how quickly the drug dissolved in the gut.
Which Drugs Are Most at Risk?
Not all medications are created equal when it comes to switching. Some are far more sensitive to tiny changes in how they’re absorbed.
- Narrow Therapeutic Index (NTI) drugs: These have a tiny window between effective and toxic. Examples: warfarin (blood thinner), levothyroxine (thyroid), phenytoin (seizure control), cyclosporine (transplant rejection). Even a 10% change in absorption can cause harm.
- Anti-epileptics: A single seizure can change a life. Studies show a higher rate of breakthrough seizures after switching generics.
- Immunosuppressants: For transplant patients, a drop in drug levels can trigger organ rejection.
- Cardiac glycosides: Like digoxin. Too little? Heart rhythm goes haywire. Too much? Toxicity.
If you’re on one of these, switching generics isn’t just about saving money-it’s a medical gamble. And not every generic is made the same. A generic made by Company A might use one excipient. The same drug made by Company B might use another. And if your pharmacy switches suppliers without telling you? You might not notice until you feel off.
How to Protect Yourself
You don’t have to accept side effects as “just part of taking meds.” Here’s how to take control:
- Ask your pharmacist. They know what’s in each pill. Ask: “Is this the same manufacturer as last time?” or “What’s the filler in this version?”
- Check the package insert. It’s often tucked inside the box. It lists all excipients-even ones you’ve never heard of. If you’re allergic to gluten, dyes, or lactose, cross-reference them.
- Request ‘Do Not Substitute’. If you’ve had a bad reaction, ask your doctor to write “Dispense as Written” on your prescription. That legally blocks the pharmacy from switching brands.
- Keep a symptom diary. Note when you switch pills. Did your headaches start? Did your energy drop? Did your seizures return? Linking timing to the switch helps you and your doctor spot patterns.
- Stick with one generic manufacturer. If you find a generic that works, try to keep getting it. Some pharmacies will let you request a specific brand of generic.
Many people don’t realize that excipient information isn’t on the pill bottle. You have to dig for it. And most pharmacies won’t volunteer it unless you ask.

The Bigger Picture
Generics save the U.S. healthcare system over $370 billion a year. That’s huge. But behind that number are real people-millions-who have food allergies, autoimmune conditions, or gut sensitivities. The FDA estimates 15-20 million Americans have significant excipient intolerances. That’s not a niche group. It’s a public health blind spot.
That’s why, in early 2024, the FDA announced plans for a public database listing excipients in both brand and generic drugs. It’s a first step. Meanwhile, some generic manufacturers are starting to market their products as “clean excipient” formulations-especially for NTI drugs.
Cost matters. But so does safety. For most people, generics are safe, effective, and the smart choice. But if you’ve ever felt “off” after switching pills-even if your doctor said it was “just in your head”-you’re not imagining it. The chemistry is real. The difference is real. And you deserve to know what’s in your medicine.
What’s Next?
By 2030, experts predict that excipient transparency will be a key selling point for generic manufacturers. Imagine choosing a generic not just by price-but by whether it’s free from dyes, lactose, or gluten. That’s not science fiction. It’s already starting.
Until then, stay informed. Ask questions. Track your symptoms. Your body knows when something’s wrong. Don’t let a hidden ingredient in a pill make you pay the price.
Can generic medications have different side effects than brand-name drugs?
Yes, but not because of the active ingredient. Generic drugs contain the same active drug as the brand, but they can use different inactive ingredients-called excipients. These can include lactose, dyes, gluten, or preservatives. If you’re sensitive to any of these, you might experience side effects like nausea, bloating, rashes, or even changes in how the drug is absorbed. These aren’t side effects of the medicine itself-they’re reactions to the filler.
Which medications are most likely to cause problems when switching to generics?
Drugs with a narrow therapeutic index (NTI) are the most sensitive. These include warfarin (blood thinner), levothyroxine (thyroid hormone), phenytoin (anti-seizure), cyclosporine (immunosuppressant), and digoxin (heart medication). Even small changes in how quickly the drug enters your bloodstream can lead to treatment failure or serious side effects. Parkinson’s medications like levodopa are also frequently reported to cause issues after switching.
How can I find out what excipients are in my medication?
The easiest way is to ask your pharmacist. They can check the manufacturer’s product information. You can also look for the package insert that comes with your prescription-it lists all inactive ingredients. Online databases like the FDA’s upcoming excipient registry will help, but right now, you need to request this info. Don’t assume it’s on the label-it usually isn’t.
Can I ask my doctor to prescribe only the brand-name drug?
Yes. If you’ve had a bad reaction to a generic, ask your doctor to write “Dispense as Written” or “Do Not Substitute” on your prescription. This legally prevents the pharmacy from switching to a generic version. Some insurance plans may require prior authorization, but if your doctor states it’s medically necessary, they usually approve it.
Are generic drugs less effective than brand-name drugs?
For most people, no. Studies show 92% of generics perform just as well as brand-name drugs. But for a small percentage of patients-especially those with excipient sensitivities or on NTI drugs-switching can lead to reduced effectiveness. This isn’t because the generic is “weaker.” It’s because the excipients changed how the drug was absorbed. If you notice your symptoms returning after a switch, talk to your doctor. It might not be your condition worsening-it might be your pill.


Maddi Barnes
February 19, 2026 AT 18:45