Antibiotic Need Calculator
Is This Infection Likely Bacterial?
Answer the following questions to see if your infection might require antibiotics. Based on CDC guidelines and stewardship principles.
Your Risk Assessment
What This Means
Every year, millions of people take antibiotics without needing them. It’s not because they’re reckless-it’s because it’s easy to assume that a bad cough or a lingering fever must be bacterial. But most sore throats, colds, and even some sinus infections are caused by viruses. And when antibiotics are used when they’re not needed, they don’t just fail to help-they hurt.
Why Antibiotics Can Do More Harm Than Good
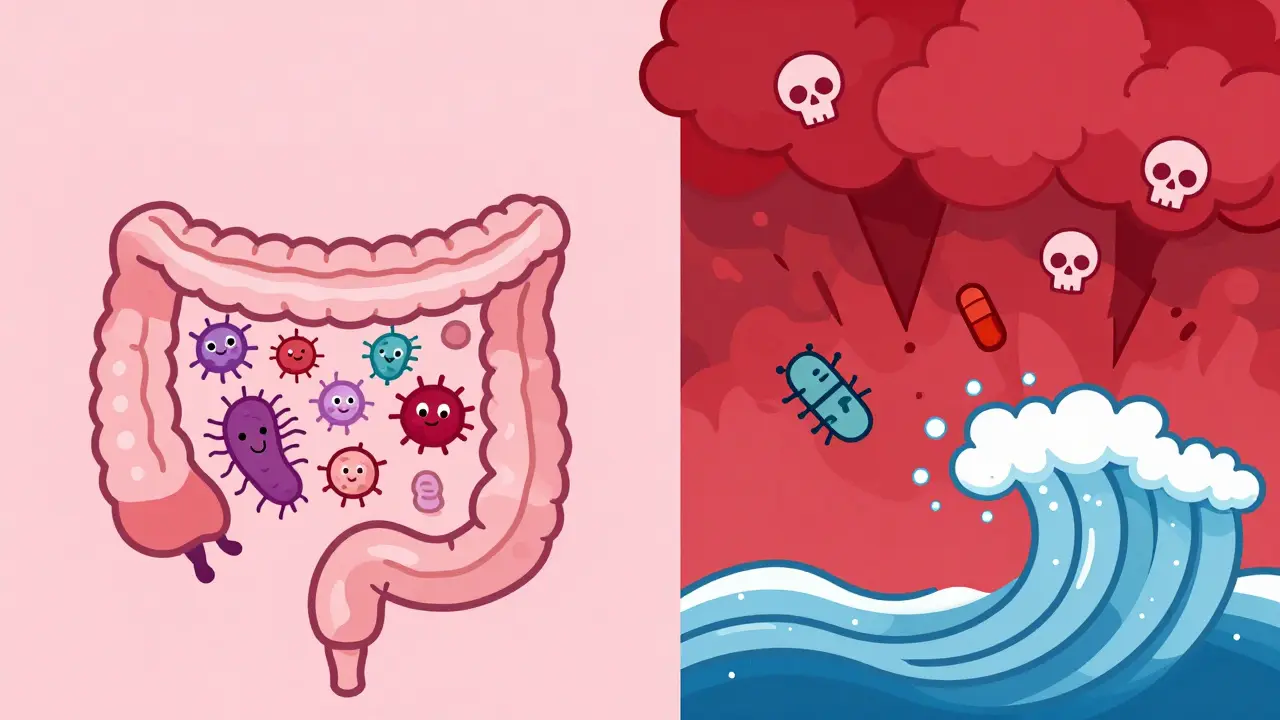
Antibiotics aren’t harmless magic pills. They’re powerful drugs designed to kill bacteria. But they don’t pick and choose. They wipe out both the bad bugs and the good ones-especially the helpful bacteria in your gut. That disruption can lead to serious side effects, the most dangerous being Clostridioides difficile (C. diff) infection. C. diff causes severe diarrhea, colitis, and in extreme cases, death. People who’ve taken broad-spectrum antibiotics are 7 to 10 times more likely to get it than those who haven’t.The CDC found that at least 30% of outpatient antibiotic prescriptions in the U.S. are unnecessary. In hospitals, it’s still 20%. That means hundreds of thousands of people each year are exposed to risks they don’t need to face. And it’s not just C. diff. Antibiotics can cause allergic reactions, kidney damage, yeast infections, and long-term changes to your microbiome that may affect your immune system for months-or even years.
What Antibiotic Stewardship Actually Means
Antibiotic stewardship isn’t about banning antibiotics. It’s about using them wisely. The formal definition from the CDC is simple: “The effort to measure and improve how antibiotics are prescribed by clinicians and used by patients.” But in practice, it’s more precise: the right drug, at the right time, in the right dose, for the right bug, and for the right duration.This isn’t theoretical. Hospitals that run stewardship programs have seen C. diff rates drop by 25-30%. Adverse drug events from antibiotics fell by over 21% across 28 U.S. hospitals in one major study. These aren’t small wins. They’re life-saving changes.
Stewardship programs use real tools: clinical pharmacists review prescriptions daily, doctors get alerts when they order broad-spectrum antibiotics for mild infections, and labs test for biomarkers like procalcitonin to tell if an infection is bacterial or viral. One study showed that using procalcitonin helped cut antibiotic use by nearly 3 days for pneumonia patients-without making outcomes worse.
How Hospitals Are Getting It Right
In large hospitals, stewardship programs are now standard. As of 2023, 88% of U.S. hospitals with over 200 beds have formal programs. That’s up from just 40% in 2014. Why? Because the data speaks for itself.Nebraska Medicine, for example, launched its program in 2004. They assigned dedicated pharmacists to review every antibiotic order in the ICU and ER. They didn’t just say “no.” They offered alternatives: narrower antibiotics, shorter courses, or even no antibiotics at all. Over time, their C. diff rates dropped by 32%. Patients had fewer complications. Staff felt more confident prescribing. And the hospital saved money.
These programs need structure. The CDC’s Core Elements framework says you need three things: leadership support, drug expertise (usually an infectious disease pharmacist), and data tracking. You also need at least 1.5 full-time staff members per hospital-half a doctor and one full-time pharmacist. It’s not cheap. Annual costs run $40,000-$60,000 per FTE. But the savings from fewer infections, shorter hospital stays, and less resistance far outweigh the cost.
The Big Barrier: Fear and Uncertainty
So why aren’t all doctors doing this? The biggest problem isn’t ignorance-it’s fear.Many clinicians worry that if they don’t prescribe a broad-spectrum antibiotic, they’ll miss something deadly. Especially in the ER or ICU, where patients are critically ill and time is short, it’s tempting to cover all bases. But that’s exactly when overuse happens. One ICU doctor put it bluntly: “Fear of pathogens not covered by empirical antibiotics drives us to use too much.”
Stewardship doesn’t mean holding back when a patient is crashing. It means starting strong, then quickly narrowing down. If a patient improves after 48 hours on a broad antibiotic, the stewardship team asks: “Can we switch to something more targeted? Can we stop it sooner?” That’s not risky-it’s smarter.
Outpatient Care Is Still Falling Behind
Hospitals are making progress. But most unnecessary antibiotics are prescribed in doctor’s offices and urgent care centers. The CDC estimates 47 million unnecessary prescriptions are written each year in outpatient settings. That’s nearly one for every adult in the U.S.Why? Because patients expect antibiotics. They’ve been told for decades that antibiotics fix everything. And doctors, under time pressure, often give in. A 10-minute visit doesn’t leave room for a detailed discussion about viruses versus bacteria.
But change is possible. One study showed that when doctors received monthly reports comparing their prescribing rates to their peers, they cut unnecessary antibiotics by 20%. When patients got clear educational materials-like posters in waiting rooms explaining why antibiotics won’t help a cold-requests for them dropped. Simple tools, used well, work.

What’s Next? AI, Diagnostics, and Long-Term Change
The future of stewardship is faster, smarter, and more data-driven. Molecular tests can now identify bacteria and their resistance patterns in hours, not days. AI tools are being tested to scan electronic records and flag inappropriate prescriptions in real time. One 2022 study found that rapid diagnostic testing reduced antibiotic use by 2.1 days for pneumonia patients-without increasing readmissions.But technology alone won’t fix this. Behavior change takes time. It takes training. It takes culture. The IDSA/SHEA guidelines say stewardship programs are most effective when led by infectious disease physicians with specialized training. That’s not just a suggestion-it’s a necessity. Pharmacists need 40 hours of focused training in antibiotic use, microbiology, and clinical decision-making.
The World Health Organization calls stewardship one of the three pillars-along with infection control and patient safety-needed to prevent a global health crisis. Without it, antimicrobial resistance could cause 10 million deaths a year by 2050. That’s not a distant threat. It’s already here.
What You Can Do
You don’t need to be a doctor to help. If you’re prescribed an antibiotic, ask:- Is this infection definitely bacterial?
- What’s the shortest course that will work?
- Are there side effects I should watch for?
- What happens if I don’t take it?
Don’t pressure your doctor. Don’t demand antibiotics for a cold. And never save leftover antibiotics for next time. That’s how resistance grows.
Stewardship isn’t about denying care. It’s about giving better care. It’s about protecting your body from the harm antibiotics can cause when they’re used carelessly. It’s about making sure these life-saving drugs still work when we really need them.
What is antibiotic stewardship?
Antibiotic stewardship is a set of coordinated strategies to improve how antibiotics are prescribed and used. The goal is to ensure patients get the right drug, at the right dose, for the right bug, and for the right length of time. It’s designed to fight antibiotic resistance and reduce harmful side effects like C. diff infections.
How does antibiotic stewardship reduce side effects?
By avoiding unnecessary antibiotic use, stewardship prevents damage to the body’s good bacteria-especially in the gut. This lowers the risk of serious side effects like C. diff infection, which can cause life-threatening diarrhea. Studies show stewardship programs reduce C. diff rates by 25-30% and cut overall adverse drug events by over 20% in hospitals.
Are antibiotics always needed for infections like sinusitis or bronchitis?
No. Most cases of sinusitis, bronchitis, and sore throats are caused by viruses, not bacteria. Antibiotics don’t work on viruses. In fact, prescribing them in these cases increases the risk of side effects without improving recovery time. Stewardship programs help doctors identify when antibiotics are truly needed and when watchful waiting is safer.
Why are hospitals better at antibiotic stewardship than clinics?
Hospitals have dedicated teams-pharmacists, infectious disease specialists, and data systems-that can monitor prescriptions in real time. Outpatient settings often lack these resources. Doctors in clinics are under time pressure, patients expect antibiotics, and there’s less oversight. But new tools like prescribing feedback reports and patient education are helping close the gap.
Can antibiotic stewardship really prevent deaths?
Yes. The CDC estimates that antibiotic resistance causes 35,000 deaths each year in the U.S. alone. Many of these deaths come from infections that no longer respond to common antibiotics. Stewardship slows resistance by reducing unnecessary use, keeping antibiotics effective for when they’re truly needed. This directly saves lives-not just from resistant infections, but also from side effects like C. diff.

Aditya Gupta
January 31, 2026 AT 16:22bro i got amoxicillin for a cold last year and it did nothing but give me diarrhea for a week. why do we still do this??
Chris & Kara Cutler
February 1, 2026 AT 04:28YES. My kid got C. diff after a 5-day course for a 'bad ear infection' that turned out to be viral. 🤢 Antibiotics aren't candy. We need to stop treating them like they are. 🙏
Donna Macaranas
February 2, 2026 AT 02:16I work in a clinic and I see it all the time. Parents ask for antibiotics like it's a favor. Doctors give in because they're tired. It's not malice-it's burnout. But we can do better.
Rachel Liew
February 4, 2026 AT 00:12my grandma died from c diff after a simple pneumonia treatment. i never knew antibiotics could do that. i always thought they were safe. this changed my whole view.
Nicki Aries
February 4, 2026 AT 20:03Every time I see a doctor, I ask: 'Is this bacterial?' And then I wait. And then I don't take the pill unless they say yes. And guess what? I haven't been sick in two years. It's not magic-it's just not poisoning myself.
Melissa Melville
February 6, 2026 AT 15:23So let me get this straight-we have a system where doctors are pressured to give out drugs they know don't work… because patients think it’s the only way to feel better? And we’re surprised when people get sicker? 😅
Naresh L
February 7, 2026 AT 17:52It’s funny how we treat antibiotics like they’re divine intervention, yet we don’t treat insulin or antivirals the same way. Why? Because we’ve been conditioned to believe bacteria are the only enemy. But the real enemy is ignorance-and profit.
franklin hillary
February 7, 2026 AT 18:34Hospitals are doing great, but outpatient is a disaster zone. I’ve had urgent care docs hand me a script for amoxicillin for bronchitis while I was still coughing into a tissue. No labs. No questions. Just 'take this.' That’s not medicine. That’s assembly-line fear-mongering.
Bob Cohen
February 9, 2026 AT 10:16My cousin is a nurse in a rural ER. She told me they get called out for 'not prescribing enough' if they don't give antibiotics. The system punishes restraint. We need to change the incentives, not just the education.
Ishmael brown
February 11, 2026 AT 00:42AI will fix this? LOL. The same AI that told my mom her rash was 'just stress' when it was Lyme? Nah. We don’t need tech-we need doctors who aren’t terrified of lawsuits.
Jaden Green
February 12, 2026 AT 02:43Let’s be real: this whole 'stewardship' movement is just Big Pharma’s way of making us feel guilty for taking the one thing that's kept us alive since the 1940s. Meanwhile, they’re patenting new antibiotics that cost $50,000 a dose. The real villain isn’t the patient who asked for a pill-it’s the corporate machine that profits from our fear.
Angel Fitzpatrick
February 12, 2026 AT 17:18They’re hiding the truth. Antibiotics are a Trojan horse. The microbiome collapse is intentional. The CDC? The WHO? All part of the Great Microbiome Depopulation Initiative. They want us weak. They want us dependent. C. diff? That’s not a side effect-it’s a feature. You think they care about your gut? They care about your insurance premiums.
Nidhi Rajpara
February 14, 2026 AT 06:03It is imperative that medical professionals receive continuous education regarding the appropriate utilization of antimicrobial agents. The prevalence of inappropriate prescriptions remains alarmingly high, and the consequences are both clinically and economically devastating. We must prioritize evidence-based practice over patient demand.