Switching from brand-name carbamazepine to a generic version might seem like a simple cost-saving move - but for many people with epilepsy or nerve pain, it can be anything but. Carbamazepine isn’t like most medications. Even small changes in how it’s absorbed or processed by your body can lead to breakthrough seizures, dangerous side effects, or treatment failure. And the reason? Its powerful effect on liver enzymes and its narrow therapeutic window.
Why carbamazepine is different
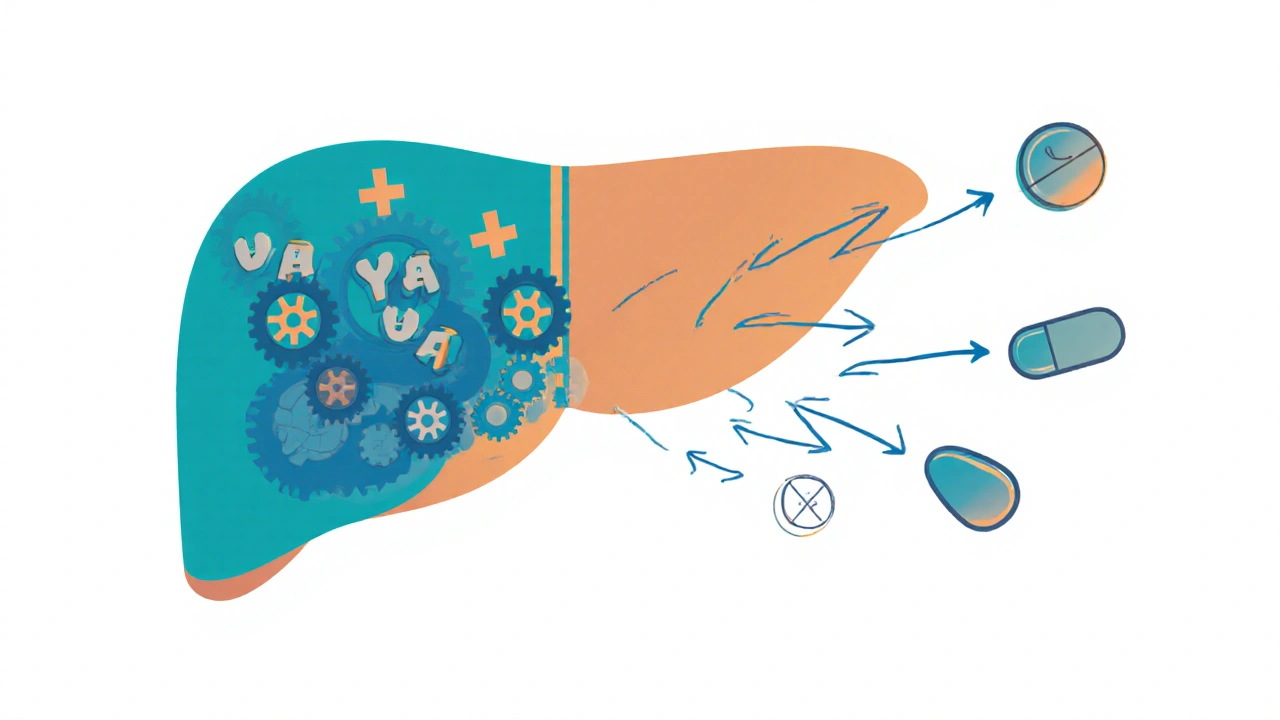
Carbamazepine works by calming overactive nerve cells in the brain, which helps control seizures and certain types of nerve pain. But here’s the catch: it doesn’t just act on your brain - it also tricks your liver into making more of the enzymes that break it down. This is called enzyme induction. Specifically, carbamazepine ramps up CYP3A4, one of the most important liver enzymes. This enzyme doesn’t just process carbamazepine - it handles about half of all prescription drugs you might be taking.That means if you’re on carbamazepine, other medications can become less effective - or even useless. Warfarin, the blood thinner, loses its punch. Cyclosporine, used after organ transplants, drops to unsafe levels. Birth control pills may fail. Even some HIV drugs and antifungals stop working as they should. The induction doesn’t happen overnight. It starts in 2-3 days, peaks around 2-3 weeks, and sticks around for up to two weeks after you stop the drug. That’s why a change in dosage or brand might not show problems right away - but they’ll come.
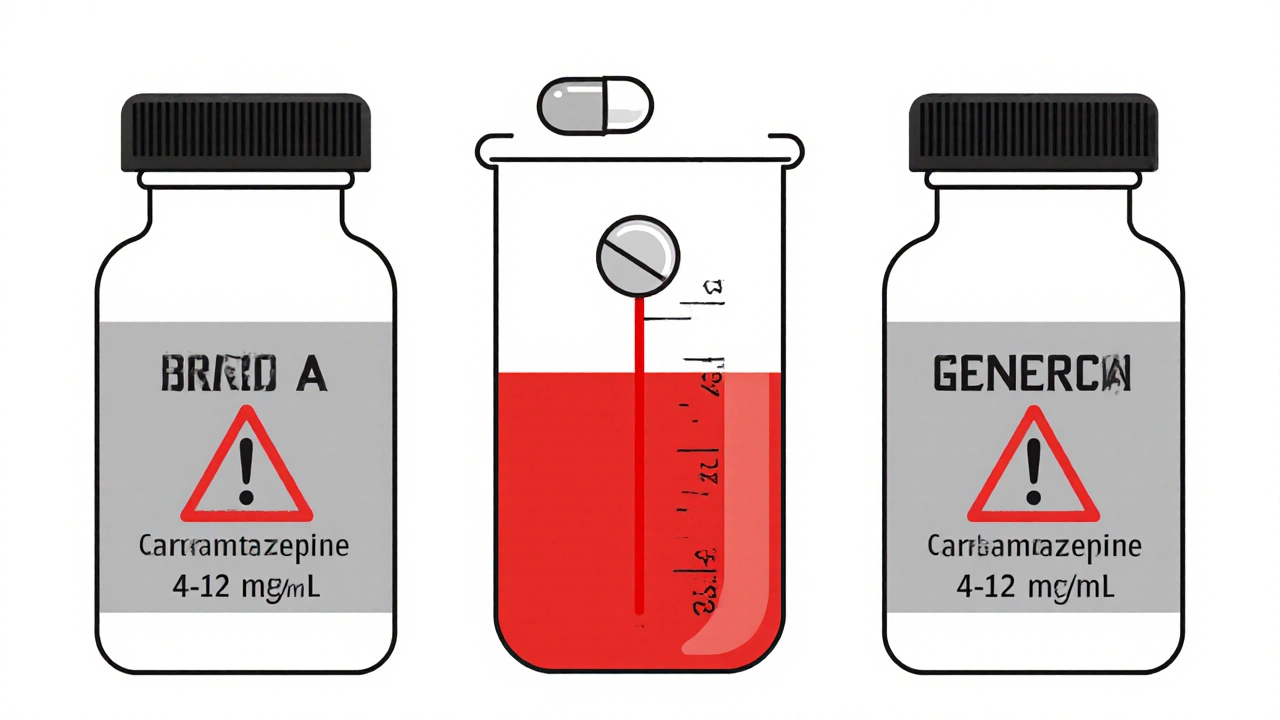
The narrow therapeutic index problem
Carbamazepine’s effective range is tiny: 4 to 12 micrograms per milliliter of blood. Go below 4, and seizures can return. Go above 12, and you risk dizziness, double vision, nausea, or even life-threatening toxicity. That’s a narrow band - and the difference between safe and dangerous can be as little as 2-3 mcg/mL.Now add another layer: people absorb and process carbamazepine very differently. One person might need 600 mg a day to stay in range. Another might need 1,200 mg. That’s why over 65% of people on carbamazepine need regular blood tests - called therapeutic drug monitoring (TDM). Without it, you’re flying blind.
And here’s where generics get risky. All generic versions must prove they’re “bioequivalent” to the brand - meaning they deliver the same amount of drug into the bloodstream within an 80-125% range. Sounds fair, right? But for a drug like carbamazepine, that 45% swing is huge. A 10% difference in absorption can push someone from 9 mcg/mL to 10.5 mcg/mL - still in range. But if you switch from one generic to another, and your level drops from 9 to 7.5, you’re now near the bottom of the therapeutic window. Seizures can return. And if you’re on multiple antiepileptic drugs, that variability jumps even higher - from 25% to 45% in some cases.
What the studies say about generic switches
A 2018 study tracked 327 patients who switched between different carbamazepine generics. Twelve percent had serious problems: seizures returned, side effects worsened, or they ended up in the ER. Nearly 8% needed emergency care. Another study found that women of childbearing age were 22% more likely to have breakthrough seizures after switching - likely because hormones affect how fast CYP3A4 works.Patients themselves are reporting this too. On epilepsy forums, people describe waking up to more seizures after a pharmacy switch. One user’s blood level dropped from 7.2 to 4.8 mcg/mL - a 33% fall - after switching to a generic. That’s not a glitch. That’s a clinical event.
Even the FDA admits there’s a problem. In 2023, they listed carbamazepine extended-release formulations as “high-priority” for better testing methods. Why? Because current bioequivalence studies use 24-36 healthy volunteers. But real patients have other illnesses, take other drugs, have liver or kidney issues, or are women on birth control - all of which change how carbamazepine behaves. A pill that works fine in a healthy 30-year-old man might not work the same in a 55-year-old woman with diabetes and high blood pressure.
Extended-release vs. immediate-release: the hidden difference
There are two main types of carbamazepine: immediate-release tablets and extended-release capsules (like Carbatrol, Tegretol XR, or Equetro). The extended-release versions release the drug slowly over time, keeping levels steadier. That’s good - less fluctuation means fewer side effects and better seizure control.But here’s the kicker: different generic manufacturers use different bead sizes, coatings, and release mechanisms. One company’s capsule might dissolve faster in the stomach than another’s - especially in people with slow digestion (gastroparesis) or who take acid-reducing meds. A 2023 study found that Nostrum Pharmaceuticals’ extended-release capsules had different bead sizes than others, causing problems in patients with digestive issues. That’s not a flaw in the drug - it’s a flaw in how we test generics.
And the FDA’s current dissolution tests? They’re done in lab conditions that don’t match real stomach pH levels. For NTI drugs like carbamazepine, that’s not enough. The EMA in Europe now requires steady-state bioequivalence studies - meaning they test patients after weeks of taking the drug, not just a single dose. The U.S. is starting to catch up, but it’s not standard yet.
Who’s most at risk?
Not everyone has trouble with generic carbamazepine. About 60% of patients switch without issue. But certain groups are far more vulnerable:- People with poorly controlled seizures - even a small dip in levels can trigger a seizure.
- Women of childbearing age - hormonal changes alter enzyme activity, making levels unpredictable.
- Patients on multiple medications - each drug competes for the same liver enzymes, making carbamazepine harder to predict.
- People of Asian descent - if you carry the HLA-B*1502 gene, carbamazepine can cause Stevens-Johnson Syndrome, a deadly skin reaction. Screening is required before starting.
- Older adults or those with liver/kidney problems - slower metabolism means drug levels build up faster.

What you should do
If you’re on carbamazepine, here’s what actually works:- Ask your doctor to write “dispense as written” or DAW 1 on your prescription. That stops the pharmacy from swapping brands without your permission.
- Know your manufacturer. Keep a note of the name on your pill bottle - Nostrum, Mylan, Teva, etc. If it changes, tell your doctor immediately.
- Get blood tests before and after any switch. Check levels at baseline, then again at 7-10 days and 4 weeks after switching. If your level drops or rises more than 15%, your dose needs adjusting.
- Don’t assume generics are interchangeable. Even if they’re both “carbamazepine,” they’re not the same pill. Think of them like different brands of insulin - same name, different behavior.
- Report any changes. More seizures? New dizziness? Rash? Tell your neurologist. These aren’t “just side effects” - they could be a sign your drug level changed.
Some neurologists now avoid switching carbamazepine altogether - especially in patients with frequent seizures or a history of adverse reactions. The American Academy of Neurology’s 2019 guidelines back this up: don’t switch unless absolutely necessary.
The future: precision dosing
The good news? Science is catching up. Researchers in Glasgow have identified 17 gene variants that affect how people process carbamazepine. People with the CYP3A4*22 variant, for example, need 25% less drug to reach safe levels. In the next five years, doctors may use genetic tests to start patients on the right dose from day one - cutting out the guesswork entirely.The FDA’s Sentinel Initiative is tracking 500,000 carbamazepine users through 2025 to see what really happens when people switch generics. And the American Epilepsy Society is building a new TDM toolkit for doctors that will factor in age, sex, weight, and other meds to predict the right dose.
For now, though, the message is clear: carbamazepine isn’t a drug you should switch lightly. Its enzyme-inducing power and narrow range make it one of the most dangerous medications to swap between generics. If you’re stable on your current version - stay on it. If you must switch, do it with blood tests, your doctor’s guidance, and full awareness of the risks.
Frequently Asked Questions
Can I switch between different carbamazepine generics without problems?
Some people can switch without issues, but many cannot. Even though generics meet FDA bioequivalence standards, small differences in how the drug is released or absorbed can cause blood levels to drop or rise enough to trigger seizures or side effects. About 12% of patients experience problems after switching, and 8% end up in the emergency room. Always check your carbamazepine blood level before and after any switch.
Why does carbamazepine affect other medications?
Carbamazepine strongly induces the CYP3A4 liver enzyme, which breaks down about half of all prescription drugs. This means medications like warfarin, birth control pills, cyclosporine, and some HIV drugs get cleared from your body faster - making them less effective. If you start or stop carbamazepine, your doctor must check all your other meds to adjust doses accordingly.
How long does it take for carbamazepine to start affecting enzyme levels?
Carbamazepine begins inducing liver enzymes within 48-72 hours of starting it. The effect builds over 2-3 weeks and peaks around that time. Even after you stop taking it, the enzyme induction can last 1-2 weeks. This means interactions with other drugs can appear days or weeks after a change - not immediately.
Do I need blood tests if I’m on a generic version?
Yes. Therapeutic drug monitoring (TDM) is recommended for 65-75% of people on carbamazepine, regardless of brand or generic. Because the therapeutic range is so narrow (4-12 mcg/mL), and because people process the drug differently, blood tests are the only way to know if you’re getting the right dose. This is especially critical after switching generics or changing doses.
Is carbamazepine safe for people of Asian descent?
Not without screening. People of Asian descent who carry the HLA-B*1502 gene have a 10-fold higher risk of developing Stevens-Johnson Syndrome - a life-threatening skin reaction - when taking carbamazepine. The FDA requires genetic testing before starting the drug in these populations. If you’re positive for this gene, your doctor should choose a different medication like levetiracetam instead.
Can I switch from extended-release to immediate-release carbamazepine?
Switching between formulations is risky and should only be done under close medical supervision. Extended-release versions (like Tegretol XR) provide steadier blood levels, reducing side effects. Immediate-release tablets cause spikes and dips in drug levels, increasing seizure risk and side effects. If you must switch, your doctor will likely lower your daily dose and monitor your blood levels closely.


Julie Roe
November 16, 2025 AT 19:58Just wanted to say I’ve been on carbamazepine for 14 years, and I switched generics three times before I learned the hard way. My neurologist didn’t even mention it could be a problem - I just kept having these weird dizzy spells and then a minor seizure. Turns out, my blood level dropped from 8.1 to 5.3 after a pharmacy swap. I didn’t even realize it was the pill until I started writing down every brand I got. Now I keep a photo of the pill on my phone. If it looks different, I call my doctor before swallowing. It’s not paranoia - it’s survival.
Also, if you’re on birth control? Don’t assume it’s still working. I got pregnant after switching generics. No one warned me.
Trust me, this isn’t just ‘people being dramatic.’ This is real.
And yes, I’ve had to switch pharmacies twice because they kept swapping my brand without asking. DAW 1 is now written in red on my prescription.
Don’t let them treat your brain like a vending machine.
Robert Merril
November 18, 2025 AT 11:50Yeah so the FDA says generics are fine but somehow every time I switch my carbamazepine I end up in the ER like a broken record
Also why is no one talking about how the dissolution tests are done in lab water with perfect pH and zero stomach acid
Real people eat pizza and take omeprazole
Also I’m 42 and have diabetes and my liver doesn’t care what the FDA says
Also I’m not a healthy 30 year old male so stop pretending I am
Also my seizures don’t care about bioequivalence percentages
Jennifer Howard
November 19, 2025 AT 17:18As a pharmacologist with 22 years in clinical research, I must emphasize that the current bioequivalence standards for narrow therapeutic index drugs like carbamazepine are scientifically indefensible. The 80–125% range was established in the 1980s for non-critical medications and has never been validated for antiepileptics. The FDA’s reliance on single-dose studies in healthy volunteers is a regulatory failure of monumental proportion. In fact, the European Medicines Agency’s requirement for steady-state pharmacokinetic studies in target populations is the only ethically and scientifically defensible approach. Until the U.S. adopts this standard, patients are being subjected to an uncontrolled, unmonitored, and ethically questionable pharmaceutical gamble. This is not a ‘cost-saving measure’ - it is a systemic abandonment of patient safety under the guise of regulatory efficiency.
Noel Molina Mattinez
November 20, 2025 AT 01:42I switched to a generic and had a seizure at work and my boss said maybe I should just stop taking it
My neurologist didn’t even check my levels
Now I have a new job and a new insurance and they won’t cover the brand
I just take it and hope
Jennie Zhu
November 22, 2025 AT 00:04There is a critical, under-discussed variable in carbamazepine pharmacokinetics: gut microbiome variability. Emerging research indicates that inter-individual differences in intestinal flora can significantly alter the absorption profile of extended-release formulations, particularly in patients with concomitant GI disorders or antibiotic exposure. This introduces an additional layer of pharmacodynamic unpredictability beyond the current bioequivalence paradigm. The current dissolution testing protocols, which do not account for microbial metabolic activity or gastric transit time modulation, are therefore inherently inadequate for NTI drugs. Until microbiome profiling is integrated into therapeutic drug monitoring protocols, the risk of unexplained therapeutic failure will persist, particularly in populations with chronic inflammatory conditions or recurrent GI infections. This is not merely a regulatory gap - it is a fundamental oversight in personalized medicine.
Kathy Grant
November 22, 2025 AT 15:28I’ve been on carbamazepine since I was 19. I’m 38 now. I’ve had three seizures in the last 15 years. All three happened within two weeks of switching generics. I used to think I was just unlucky. Turns out, I was just unheard.
I remember one time I called my pharmacy to ask why my pill looked different. They said, ‘It’s the same thing.’ I said, ‘But it’s not the same pill.’ They laughed.
I stopped trusting pharmacies. I started keeping a notebook. Brand. Lot number. Date. Blood level. Symptoms.
It took me years to find a neurologist who didn’t roll their eyes when I brought it up. She’s the one who taught me about DAW 1. Now I print it out and hand it to the pharmacist. Sometimes they sigh. Sometimes they don’t care. But I keep doing it.
Because if I don’t, I might not wake up.
I don’t want to be a statistic. I want to be here. For my daughter. For my dog. For the quiet mornings when I don’t feel like my brain is trying to short-circuit.
So if you’re reading this and you’re on carbamazepine - don’t wait for a seizure to learn this lesson. Write DAW 1. Know your pill. Ask for the test. You’re not being difficult. You’re being smart.
Dave Feland
November 22, 2025 AT 19:41Let’s be honest - this isn’t about bioequivalence. It’s about the pharmaceutical-industrial complex colluding with the FDA to push generics so they can profit while patients become test subjects. The 2023 FDA ‘high-priority’ designation? A PR stunt. The Sentinel Initiative? A PR stunt. They’ve known this for decades. The same companies that make the brand-name drug own the largest generic manufacturers. The ‘different bead sizes’? Not an accident. It’s designed to force patients into a cycle of monitoring, doctor visits, and blood tests - all billable. The real danger isn’t the pill. It’s the system that lets them get away with it. And no one in power will ever fix it because they’re part of it.
Roberta Colombin
November 23, 2025 AT 02:07Thank you for writing this. I’m a nurse and I’ve seen too many patients come in confused, scared, and angry after a switch they didn’t consent to. I always tell them: your brain matters. Your safety matters. Your voice matters. If your pill looks different, ask. If your doctor doesn’t listen, find one who does. You are not being difficult. You are not overreacting. You are standing up for your life. And that’s brave.
Also - if you’re a woman, especially if you’re on birth control or pregnant - please, please, please get your levels checked. Hormones and carbamazepine are a dangerous dance. I’ve seen too many babies born to moms who thought their meds were fine.
You are not alone. We are here. We see you.