Imagine rolling over in bed in the morning and suddenly the room spins like a washing machine. You grab the headboard, feel nauseous, and wonder if you’re having a stroke. This isn’t rare. In fact, BPPV is the most common cause of vertigo you’ve never heard of. It doesn’t come with numbness, slurred speech, or weakness - just that terrifying, sudden spin triggered by your own head movement. And the good news? It’s not dangerous. It’s also one of the easiest conditions to fix - if you know what to do.
What Exactly Is BPPV?
BPPV stands for Benign Paroxysmal Positional Vertigo. Let’s break that down. Benign means it’s not life-threatening. Paroxysmal means it comes in sudden, short bursts. Positional means it’s tied to head movement. And vertigo? That’s the spinning feeling - like you’re on a merry-go-round when you’re perfectly still. This isn’t dizziness from low blood sugar or dehydration. This is your inner ear sending the wrong signal. Inside your ear, there are tiny calcium crystals called otoconia. Normally, they sit safely in a part of the ear called the utricle, helping you sense gravity and straight-up movement. But sometimes, they get loose. They drift into one of the three fluid-filled semicircular canals - tubes that detect head rotation. When you move your head, these loose crystals jiggle the fluid, tricking your brain into thinking you’re spinning. Your eyes dart involuntarily (that’s nystagmus), your body feels off-balance, and nausea hits. The posterior canal gets hit 80-90% of the time. That’s why rolling over in bed, looking up at a shelf, or bending down to tie your shoes can trigger it. The symptoms last seconds, not hours. You feel fine between episodes. That’s why so many people dismiss it as ‘just getting older’ or ‘a bad night’s sleep.’Who Gets BPPV - And Why?
It’s not random. BPPV hits people over 50 most often. Women are 1.5 to 2 times more likely to get it than men. About 1 in 5 people who go to a doctor with dizziness actually have BPPV - and many more go undiagnosed. The exact reason crystals come loose isn’t always clear. Sometimes it’s after a head injury - even a minor bump. Sometimes it’s linked to inner ear infections. But in most cases, it’s just aging. Over time, the otoconia break down naturally. Think of it like sand falling out of a broken hourglass. Your body doesn’t always clean it up efficiently. You’re also more at risk if you’ve had BPPV before. About 15% of people have another episode within a year. After five years, it’s over one in three. After ten? Half of people will get it again.How Do You Know It’s BPPV - And Not Something Worse?
This is where most people get stuck. Doctors often misdiagnose BPPV. Studies show up to 35% of cases in primary care are labeled as something else - vestibular neuritis, Meniere’s disease, even anxiety. The problem? Many providers don’t know how to test for it. The real giveaway? Timing and triggers. If your spinning lasts less than a minute and only happens when you change head position, it’s likely BPPV. If you’re dizzy all day, with ringing in your ears or hearing loss, it’s probably Meniere’s. If you have numbness, double vision, or trouble walking, it could be neurological - and needs urgent attention. The gold standard test is the Dix-Hallpike maneuver. Your doctor sits you up, then quickly lowers you back while turning your head. If you have BPPV, you’ll feel the spin within 2-10 seconds, and your eyes will jump in a specific pattern. That’s nystagmus - and it’s the smoking gun. No MRI needed. No blood tests. Just a quick, simple movement.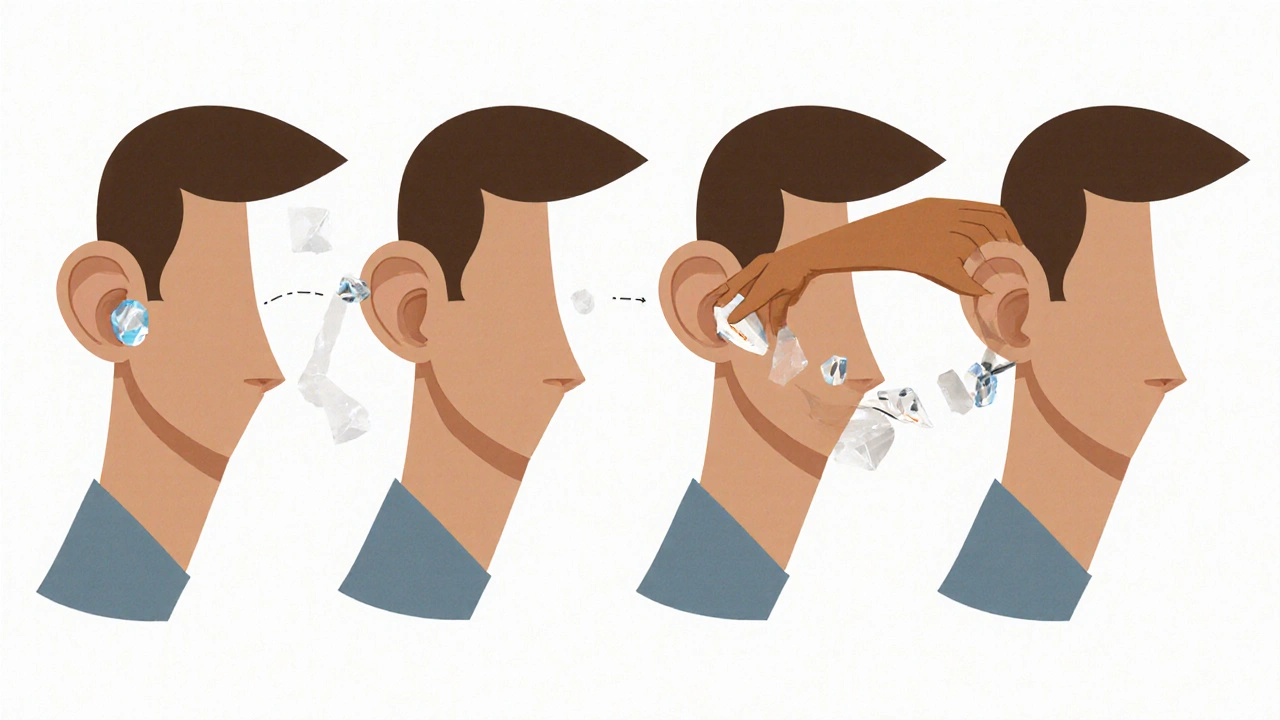
Canalith Repositioning: The Real Treatment
Here’s the truth: pills won’t fix this. Medications like meclizine or Dramamine only dull the nausea. They don’t move the crystals. And they don’t stop the spinning. In fact, they can delay recovery by masking symptoms so your brain doesn’t relearn balance. The only proven cure is moving the crystals back where they belong. That’s canalith repositioning. The most famous version? The Epley maneuver. The Epley maneuver is a series of four head positions. Each one uses gravity to guide the loose crystals out of the semicircular canal and back into the utricle, where they can be reabsorbed. It takes about 10 minutes. Most people feel better right away. Some feel a little dizzy during the procedure - that’s normal. The success rate? 80-90% after one session. There are other maneuvers too. The Semont maneuver is faster but requires more body movement. The Lempert roll is used for horizontal canal BPPV - which is rarer but causes side-to-side spinning when you lie down. The key? Precision. If you do it wrong, the crystals just move to another canal - and now you’ve got a different kind of vertigo. That’s why many people turn to YouTube videos. Over 15 million views exist for Epley maneuver tutorials. But here’s the catch: 12% of people who try it themselves say it made things worse. Why? Because they didn’t hold each position long enough, or turned their head too fast, or missed the correct ear.Can You Do It at Home?
Yes - but only if you’re sure it’s BPPV. If you’ve had the Dix-Hallpike test confirmed by a professional, then a home Epley is safe and effective. Studies show that when people follow a video guide, they have a 72% success rate. With just written instructions? Only 45%. Here’s the basic home Epley steps:- Start sitting upright on a bed. Turn your head 45 degrees toward the affected side (the side that triggers dizziness).
- Quickly lie back, keeping your head turned. Stay there for 30 seconds - or until the spinning stops.
- Turn your head 90 degrees to the opposite side, without raising it. Hold for 30 seconds.
- Roll onto your side, so you’re looking at the floor. Hold for 30 seconds.
- Sit up slowly, keeping your head slightly bent forward.
What If It Doesn’t Work?
If you’ve tried the Epley maneuver twice and still feel dizzy, it might not be BPPV - or you might have a different type. Horizontal canal BPPV, for example, needs a different maneuver. Or maybe the crystals are stuck to the canal wall (cupulolithiasis), which takes longer to clear. Your doctor might suggest the Brandt-Daroff exercises. These are done at home, twice a day for two weeks. They’re less effective - only about 50% success - but they help if you can’t access a specialist. In rare cases, if nothing works, a specialist might use a rotating chair (like the Epley Omniax) that precisely controls head movement. It’s expensive - over $75,000 - and only found in major hospitals.
Can You Prevent BPPV?
Not completely. But some research suggests vitamin D deficiency might increase your risk. If you’re over 50 and have had BPPV, ask your doctor about checking your vitamin D levels. One 2022 study showed taking 1,000 IU daily cut recurrence by 24% over a year. Also, avoid sleeping on the affected side for a few days after treatment. Some experts recommend keeping your head slightly elevated with an extra pillow for a week. Don’t do headstands. Avoid lying flat if you can help it.What Happens If You Ignore It?
BPPV doesn’t cause permanent damage. Your brain will eventually adapt. But that doesn’t mean you should wait it out. People who don’t treat it often develop a fear of movement. They stop turning their heads. They avoid stairs. They stop driving. They isolate themselves. A survey of BPPV patients found 74% were afraid of falling. 62% stopped driving. 58% skipped social events. The longer you wait, the more your balance system weakens. And the more likely you are to fall - especially if you’re older. Falls in people over 65 are the leading cause of injury-related death. BPPV might not kill you - but the fear it causes might.Why This Matters
BPPV is cheap to fix. It doesn’t need drugs, scans, or surgery. But it does need someone who knows how to test for it and how to move the crystals. Right now, 54% of patients say their doctor didn’t know how to do the maneuver. That’s why it takes an average of 3.2 months to get diagnosed. The cost? In the U.S. alone, BPPV leads to 5.6 million doctor visits a year - and $1.2-1.8 billion in unnecessary tests. Most of those are MRIs - which don’t help at all. One MRI for BPPV costs $1,200-$1,800. The Epley maneuver? $0 if you do it yourself. $50 if your clinic does it. This isn’t just about vertigo. It’s about access. It’s about knowing that a spinning room isn’t a mystery - it’s a mechanical problem. And it’s fixable.Is BPPV dangerous?
No, BPPV is not dangerous. It’s called "benign" because it doesn’t cause brain damage, stroke, or long-term health problems. But it can increase your risk of falling, especially if you’re older. The real danger is ignoring it and developing a fear of movement - which can lead to isolation, inactivity, and injury.
Can BPPV go away on its own?
Yes, BPPV can resolve on its own, usually within a few weeks. But waiting means living with dizziness, nausea, and fear. Studies show the Epley maneuver works in 80-90% of cases after one session. Waiting a month for natural recovery means 3-4 weeks of discomfort. Why suffer longer than needed?
How do I know which ear is affected?
Lie down quickly on one side. If you feel dizzy, that’s likely the affected side. If you feel dizzy on both sides, you may have BPPV in both ears - which happens in about 20% of cases. The Dix-Hallpike test is the only reliable way to confirm. If you’re unsure, see a provider trained in vestibular diagnostics.
Can I use the Epley maneuver if I have neck or back problems?
If you have severe neck arthritis, spinal fusion, or recent injury, the standard Epley maneuver may be risky. Ask your doctor about modified versions or alternatives like the Semont maneuver, which requires less neck flexion. Never force your head into a painful position.
Why do I feel dizzy during the Epley maneuver?
That’s normal. The maneuver moves the crystals, which triggers the same vertigo you’ve been feeling. The dizziness usually lasts less than a minute. If it lasts longer or you feel sick afterward, you may be doing it too fast. Slow down. Hold each position for a full 30 seconds. The goal is to let gravity do the work - not force.
If you’ve been told you have vertigo and your doctor didn’t test you with the Dix-Hallpike maneuver, ask for it. If you’ve been prescribed meclizine and still feel dizzy, ask if canalith repositioning is an option. You don’t need to live with spinning rooms. The fix is simple. It’s just not widely known.




Kathryn Ware
November 16, 2025 AT 20:12OMG I had BPPV last year and thought I was dying 😭 I went to three doctors before one actually did the Dix-Hallpike. The Epley maneuver felt like my brain was doing backflips but IT WORKED. I did it at home with a YouTube video and now I can roll over without screaming. Also, vitamin D? My levels were trash. Took 1000 IU daily and haven’t had a recurrence in 10 months. If you’re dizzy and your doc just hands you meclizine, run. Not all dizziness is anxiety. 💪
kora ortiz
November 17, 2025 AT 07:58You don’t need an MRI you don’t need drugs you don’t need to suffer. Just move the crystals. The Epley maneuver is free and 90 percent effective. Stop wasting money and time. If your doctor doesn’t know this basic thing they’re not qualified to treat vertigo. Period. Do it yourself. Watch the video. Hold each position 30 seconds. Done. No excuses.
Jeremy Hernandez
November 18, 2025 AT 07:48Lmao another wellness guru pushing the Epley like it’s some secret government cure. Who funded this article? Vestibular device companies? The real reason BPPV is misdiagnosed is because big pharma doesn’t make money off gravity. They want you on meclizine for life. And don’t even get me started on vitamin D - that’s just a placebo trick to make you feel better while the real cause is EMF exposure messing with your inner ear crystals. I’ve seen it. 2000 people in my neighborhood had this after 5G rollout. The system doesn’t want you to know.
Tarryne Rolle
November 18, 2025 AT 10:27It’s fascinating how we reduce a complex physiological phenomenon - the body’s attempt to recalibrate its relationship with gravity - to a mechanical fix. We call it ‘crystals’ like they’re little marbles, when in truth they’re symbolic of our disconnection from natural rhythms. The Epley maneuver is just a band-aid on the existential vertigo of modern life. We’ve forgotten how to be still. We spin ourselves into dizziness with screens, stress, and speed. Maybe the real cure isn’t moving crystals… but stilling the mind.
Kyle Swatt
November 18, 2025 AT 17:23Man I used to think vertigo was just ‘getting old’ until I had my first episode after a bad yoga session. Felt like the universe flipped upside down and my ears were laughing at me. The Epley? Holy hell. It’s like your brain gets a reset button. I did it three times before it clicked. And yeah - I cried during the second one. Not from pain. From relief. Like my body finally said ‘hey dumbass, I’ve been trying to tell you this for weeks.’ No pills. No scans. Just gravity and patience. That’s the real magic. And if you’re scared to do it yourself? Find someone who’s done it. Someone who gets it. You don’t need a PhD to fix your inner ear. You just need a little trust in your own body.
Deb McLachlin
November 20, 2025 AT 01:50Thank you for this comprehensive and clinically accurate overview. The emphasis on the Dix-Hallpike maneuver as the diagnostic gold standard is particularly important, as misdiagnosis remains alarmingly prevalent in primary care settings. The distinction between canalithiasis and cupulolithiasis is also underappreciated in public discourse. I would only add that while home Epley maneuvers are effective, patient selection is critical - those with cervical spine pathology or severe osteoporosis require modified protocols. The NIH trial data on DizzyFix is encouraging but limited by sample size. Further randomized controlled trials are warranted to assess long-term adherence and recurrence rates in diverse populations.
saurabh lamba
November 22, 2025 AT 00:02Bro this is just a scam. Everyone gets dizzy. You think crystals are moving? Nah. Your brain is just tired from too much chai and scrolling. I did the Epley once and felt worse. Now I just drink ginger tea and sleep on my back. No need for all this fancy stuff. People make money off fear. 😎
Kiran Mandavkar
November 23, 2025 AT 08:08How can you be so naive? You’re treating a symptom as if it were a mechanical glitch. This isn’t physics - it’s metaphysics. The otoconia are not just calcium carbonate - they’re the physical manifestation of your unresolved emotional trauma. The Epley maneuver? A colonialist attempt to ‘fix’ the body without addressing the spiritual dislocation of modernity. You think a YouTube video can heal what decades of capitalism and alienation have broken? Wake up. The real treatment is meditation. Or fasting. Or both. And stop believing in pharmaceutical-approved ‘cures’ - they’re designed to keep you dependent.