Warfarin-Antibiotic Safety Checker
Check Antibiotic Safety with Warfarin
When you’re on warfarin, even a simple course of antibiotics can turn dangerous. It’s not about the antibiotic being strong or weak-it’s about how it interacts with your blood thinner. A routine prescription for a sinus infection or urinary tract infection can send your INR soaring, putting you at risk for internal bleeding, stroke, or worse. This isn’t rare. In fact, antibiotics and warfarin interactions cause nearly one in three warfarin-related hospitalizations in older adults. And most of these are completely preventable.
Why Antibiotics Mess With Warfarin
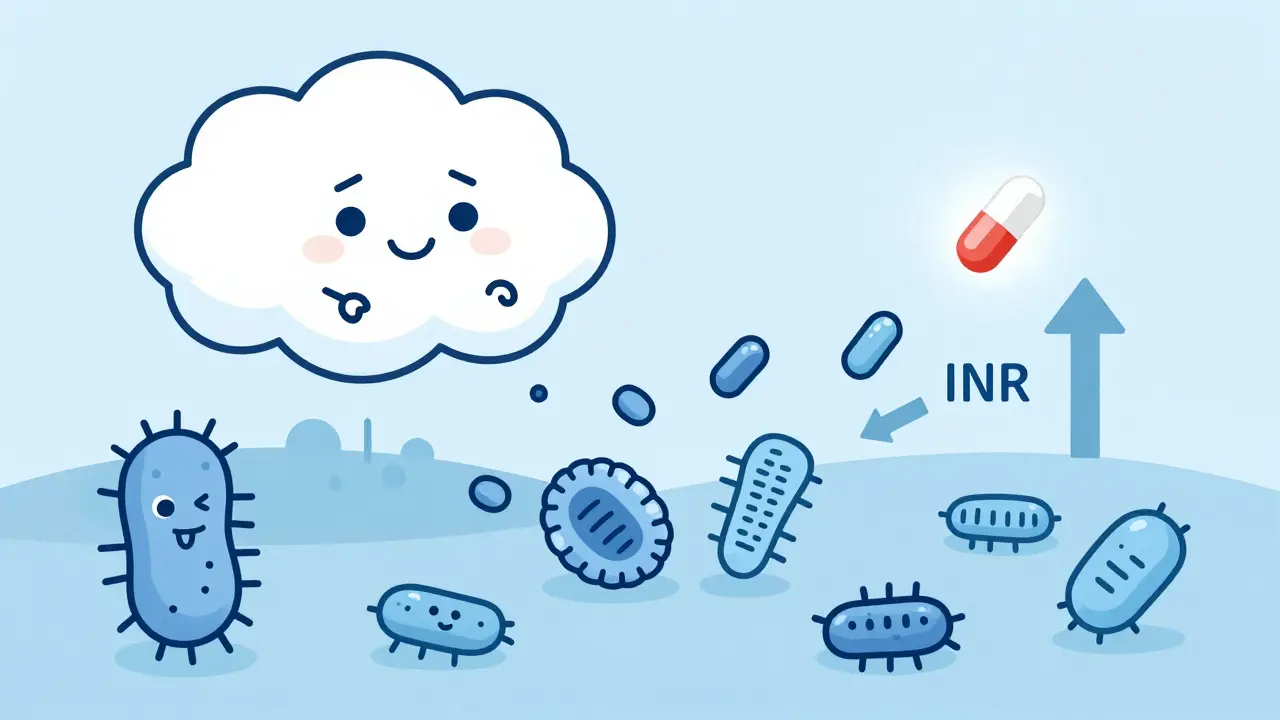
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. But your gut bacteria also make about 10-15% of your vitamin K. When you take certain antibiotics, they kill off those helpful bacteria. That means less vitamin K, more warfarin effect, and a rising INR. This usually shows up 5 to 7 days after starting the antibiotic. Then there’s the liver. Warfarin is broken down by enzymes called CYP450, especially CYP2C9. Some antibiotics block this enzyme, making warfarin stick around longer in your blood. That’s why INR can jump within 48 hours of starting drugs like ciprofloxacin or Bactrim. It’s not one mechanism-it’s two, happening at different times, which is why the risk lasts longer than you’d expect.Which Antibiotics Are Most Dangerous?
Not all antibiotics are created equal when you’re on warfarin. Some are high-risk. Others are safer. Here’s what the data shows:- High risk (INR spikes +2 or more): Ciprofloxacin, levofloxacin, erythromycin, sulfamethoxazole/trimethoprim (Bactrim), amoxicillin/clavulanate, cefotetan, cefoperazone
- Moderate risk (INR spikes +0.5 to +1.5): Azithromycin, ampicillin, ceftriaxone
- Low risk (minimal INR change): Nitrofurantoin, fosfomycin, tedizolid, penicillin V
What Happens When INR Goes Too High?
Your target INR is usually between 2.0 and 3.0. If you’re on warfarin for a mechanical heart valve or recurrent clots, it might be 2.5 to 3.5. But once your INR hits 4.0, your risk of major bleeding jumps 4 to 8 times. That means:- Unexplained bruising, especially on your arms or legs
- Bleeding gums when brushing your teeth
- Red or dark urine
- Black, tarry stools
- Headaches, dizziness, or confusion (possible brain bleed)
- Prolonged bleeding from cuts or nosebleeds
How to Stay Safe: The Real-World Protocol
There’s no guesswork here. If you’re on warfarin and your doctor prescribes an antibiotic, here’s what you need to do:- Check your INR before starting the antibiotic. Know your baseline.
- Get your INR checked within 72 hours of starting the antibiotic. Especially if it’s ciprofloxacin, Bactrim, or amoxicillin/clavulanate.
- Continue checking every 2-3 days for the first week. Even if you feel fine.
- Keep checking for 7-10 days after stopping the antibiotic. Gut bacteria take time to recover. INR can still climb after you finish the pills.
- Don’t adjust your warfarin dose yourself. Your anticoagulation clinic will decide if you need a reduction. For high-risk antibiotics like ciprofloxacin, they might lower your dose by 20-30% right away.
What About Rifampin?
Rifampin is the opposite problem. Instead of raising INR, it crashes it. This antibiotic speeds up how fast your liver breaks down warfarin. INR can drop below 1.5 in just 72 hours. That’s not just risky-it’s dangerous. You could develop a clot in your leg, lung, or brain. If you’re prescribed rifampin for tuberculosis or a stubborn infection, your warfarin dose will likely need to go up by 50-100%. You’ll need daily INR checks until your levels stabilize. Don’t assume your usual dose still works. This interaction is powerful and fast.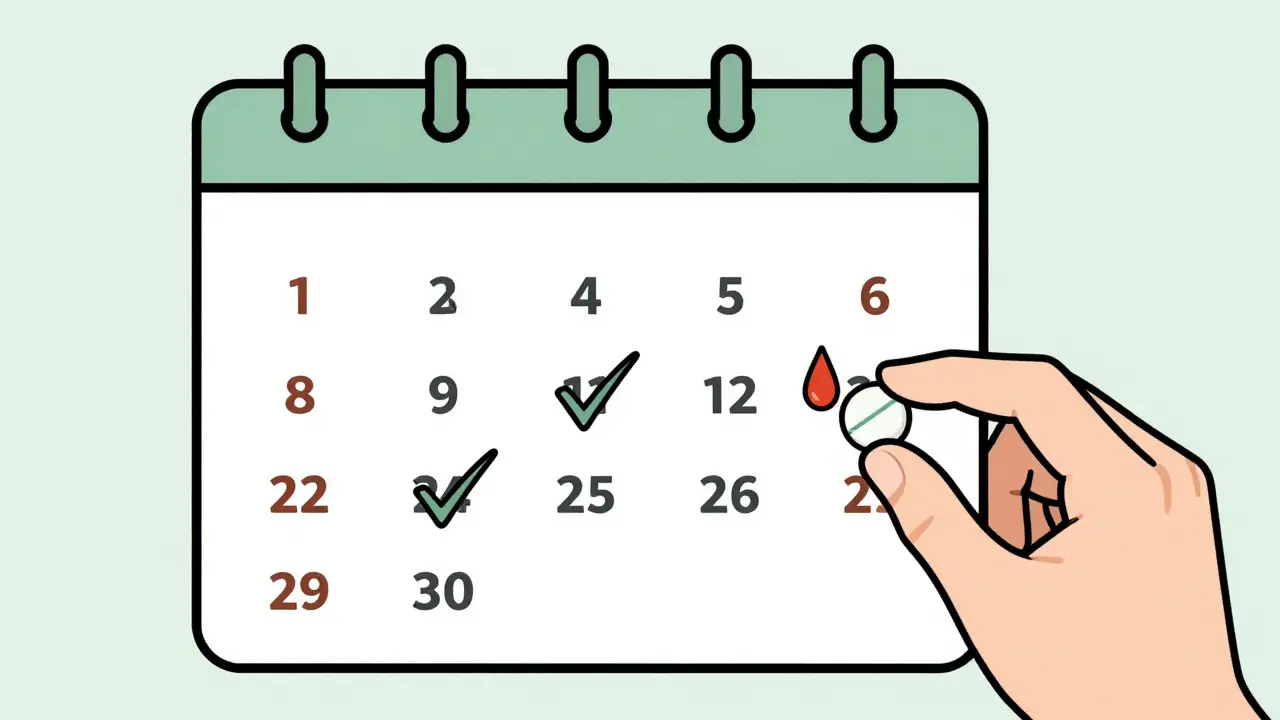
What You Can Do Right Now
If you’re on warfarin:- Keep a list of all your meds-prescription, OTC, and supplements-and show it to every doctor or pharmacist.
- Ask: “Is this antibiotic safe with warfarin?” before filling the prescription.
- Know your INR target and what your last number was.
- Set phone reminders for INR checks during and after antibiotic treatment.
- Call your anticoagulation clinic immediately if you notice unusual bleeding.
What’s Changing in 2026?
New research is pushing care forward. A 2022 study found that people with CYP2C9*2 or *3 gene variants have 2.4 times greater INR spikes when taking antibiotics. That means genetic testing could one day predict who’s at highest risk. The 2023 WARF-GEN trial showed that using genetic data to adjust warfarin doses before antibiotics reduced INR instability by 41%. That’s huge. In the next few years, we may see routine CYP2C9 testing for patients starting long-term warfarin. For now, though, the best tool is still the INR test. It’s cheap, fast, and accurate. No gene test replaces the need to monitor.Final Takeaway
Antibiotics and warfarin don’t mix safely by accident. Every time you take one, your blood’s clotting ability is being rewired-sometimes in ways you can’t predict. The good news? You don’t need to avoid antibiotics. You just need to be smarter about them. If you’re on warfarin, treat every antibiotic like a potential red flag. Check your INR before, during, and after. Talk to your anticoagulation team. Don’t wait for bleeding to happen. Prevention isn’t optional-it’s the only thing that keeps you alive.Can I take amoxicillin while on warfarin?
Amoxicillin alone is usually low risk, but amoxicillin/clavulanate (Augmentin) can raise INR by about 1.2 units on average. Always check your INR before and 72 hours after starting it. Don’t assume it’s safe just because it’s a common antibiotic.
How long after stopping an antibiotic should I keep checking my INR?
For antibiotics that kill gut bacteria (like cefotetan or amoxicillin/clavulanate), keep checking INR for 7-10 days after stopping. Vitamin K production takes time to recover. For CYP-inhibiting antibiotics like ciprofloxacin, check for 3-5 days after stopping, since enzyme effects reverse faster.
Is azithromycin safe with warfarin?
Yes, azithromycin is one of the safest antibiotics to use with warfarin. Studies show it causes only a 1.2-fold increase in bleeding risk-much lower than erythromycin or ciprofloxacin. Still, check your INR once after starting it as a precaution.
Why does my INR keep rising even after I finish my antibiotics?
Antibiotics that kill gut bacteria reduce vitamin K production, and your gut flora can take up to 10 days to bounce back. This means your INR can continue climbing after you stop the antibiotic. That’s why monitoring must continue for a full week after treatment ends.
Can I use over-the-counter painkillers while on warfarin and antibiotics?
Avoid NSAIDs like ibuprofen or naproxen-they increase bleeding risk on their own. Use acetaminophen (paracetamol) instead, but don’t exceed 3,000 mg per day. Even acetaminophen can slightly raise INR in high doses or with prolonged use, so monitor if you’re taking it long-term.